Mental Well-Being
Mental Well-Being
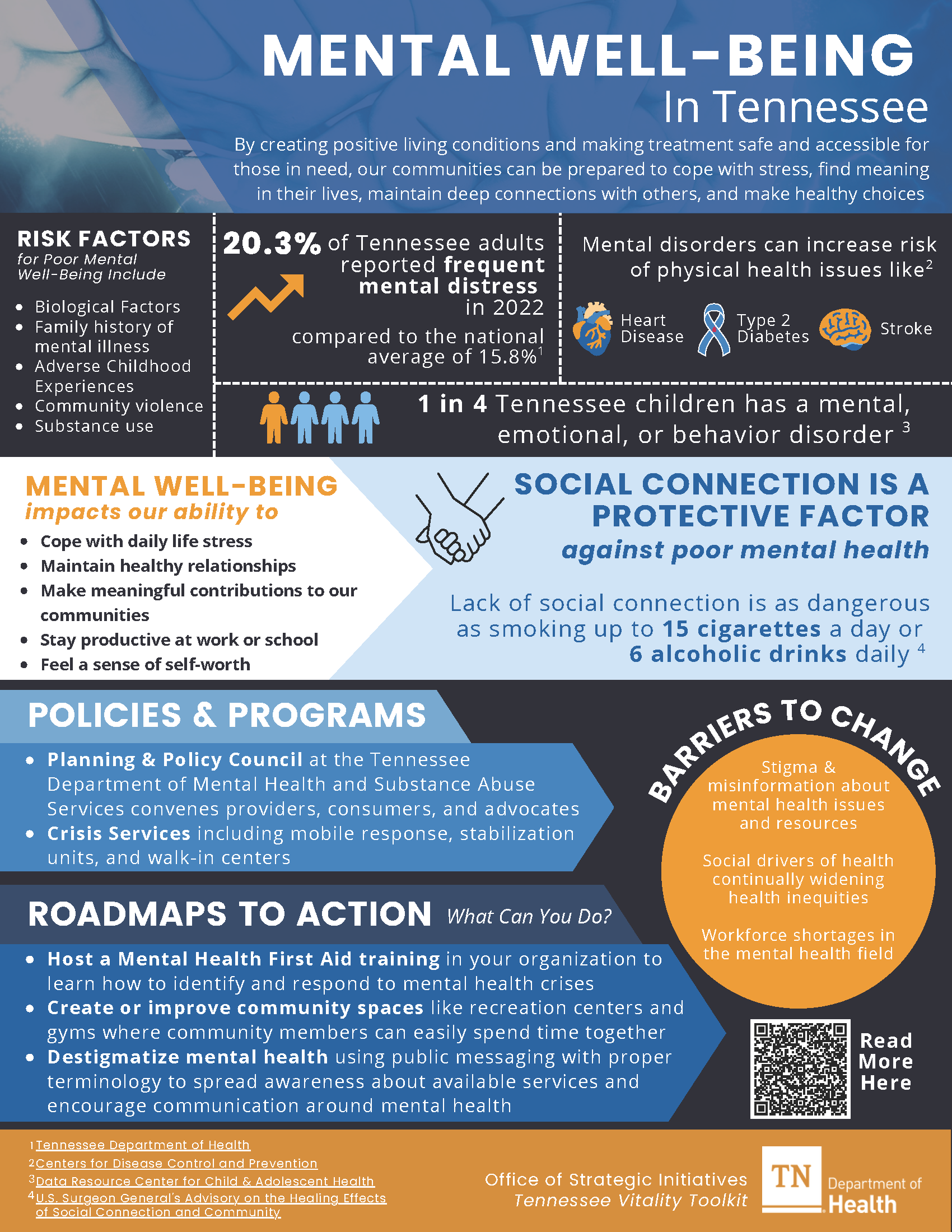
Across Tennessee, the United States, and the world, people have been facing increasing challenges with their mental health and well-being. Mental health affects how we handle stress, connect with others, make healthy choices, and live our daily lives. Good mental health is not just about surviving—it is about thriving. It means finding purpose in what we do, working to improve ourselves, and feeling good about who we are.1
Taking care of your mental well-being is as important as your physical well-being. Even if you do not have a specific mental health condition, you may still face problems that affect your well-being. It is essential to care for our mental health all the time, not just during a crisis. We can also work to create communities where everyone can do well.
Many things can affect our mental health, such as: 2
- Our biology and genetics
- Life experiences like trauma or abuse
- Family history of mental health problems
- Growing up with specific challenges, like having a parent with a mental illness
- Living with long-term medical problems like cancer or diabetes
- Facing community problems like violence or poverty
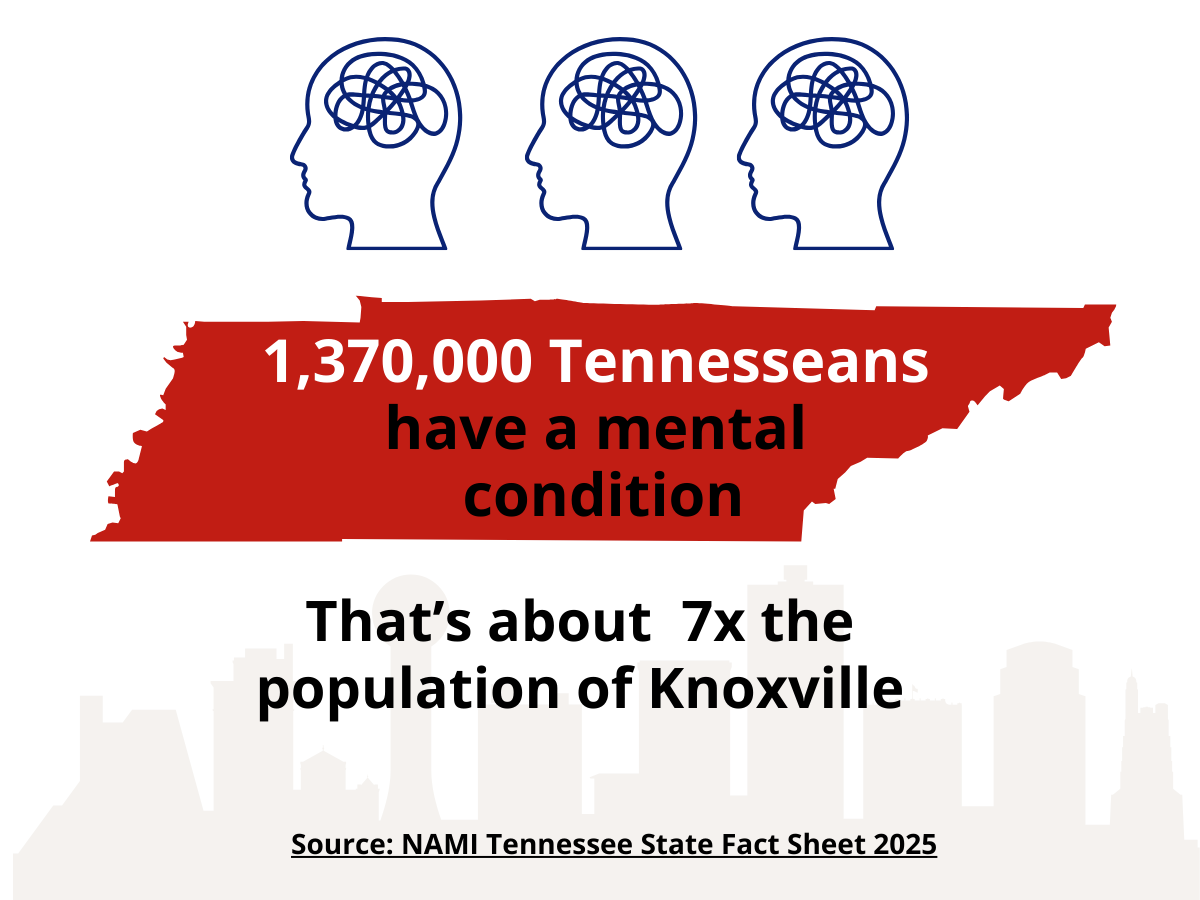
According to the American Psychiatric Association, mental illness refers to health conditions that can affect a person’s mood, thoughts, and behaviors.3 Examples include depression, anxiety, schizophrenia, eating disorders, and addictions. In the United States, mental illnesses are among the most common health conditions.4
In Tennessee:
- One in five adults (20.3%) reports frequent mental distress, compared to 15.8% nationally.5
- The 2023 suicide rate was 17.9 per 100,000, higher than the national average of 14.1 per 100,000.6
- In 2021, 42.2% of Tennessee high school students experienced Hopelessness.5
- 95.8% of counties do not have enough mental health professionals.5
Communities must focus on two main priorities when addressing mental health and well-being. First, ensure struggling people get the help and resources they need to improve. Second, create and improve community conditions, such as access to care, healthy social environments, and support for basic needs, to prevent mental distress and promote well-being in our communities.
-
Why is Mental Well-Being Important for Community Well-Being?
The community around us shapes our mental well-being and how we deal with problems. Our neighborhood, jobs, and accessible and affordable healthcare can affect how we handle everyday stress. They can even have an impact on the intensity and frequency of psychotic episodes we experience. We can reduce mental health challenges in our communities by improving community conditions, things in our daily lives that affect our well-being, and by providing high-quality mental health services.7
Mental well-being is essential for many reasons. It can help us with:8
- Coping with life’s stresses
- Building and keeping healthy relationships
- Making meaningful contributions to our community
- Staying productive at work or school
- Feeling confident and valued
Mental health can also impact your physical health. Mental disorders can increase your risk of severe health conditions like stroke, type 2 diabetes, heart disease, and more. People who struggle with their mental health may turn to drugs or alcohol to cope, which can make both their psychological and physical health worse.1
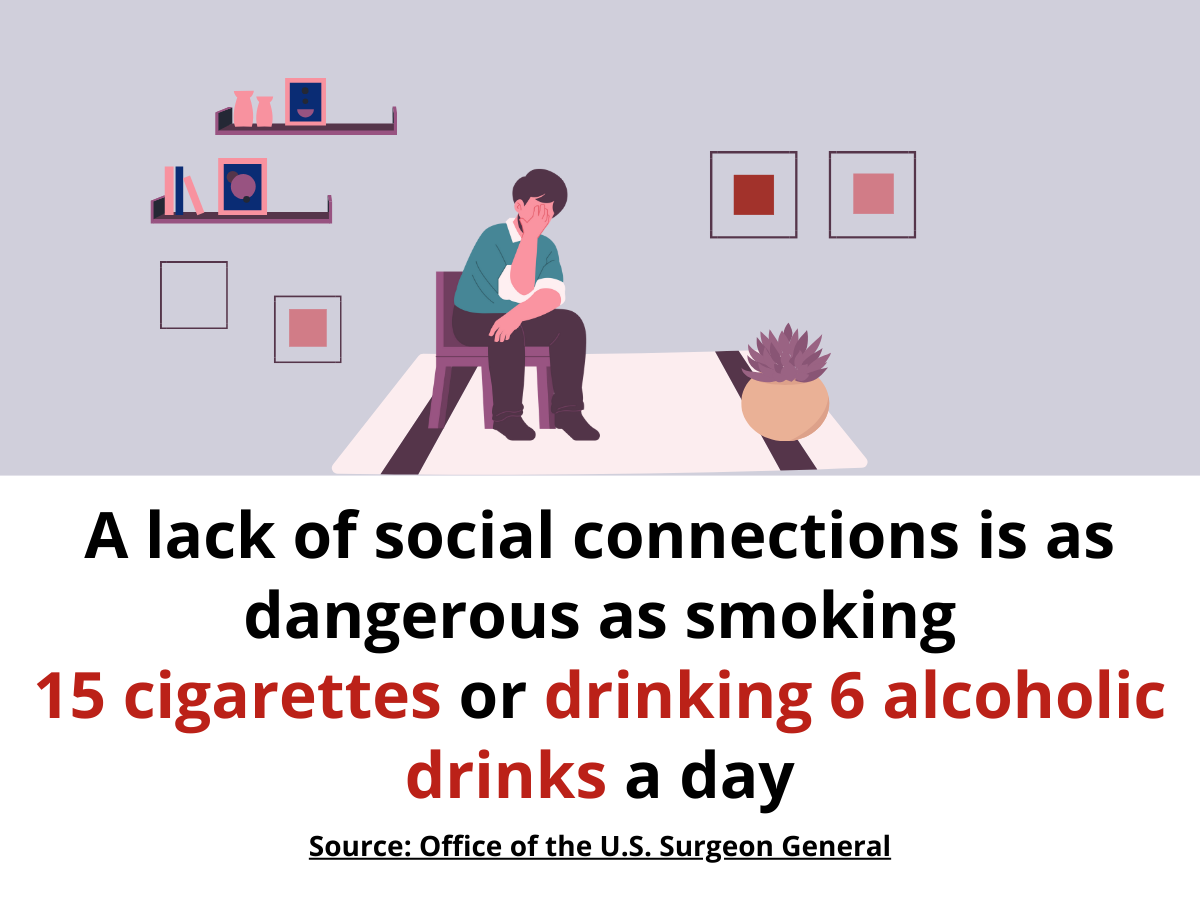
Luckily, we can strengthen our mental well-being and help others do the same through strong relationships and connections with family, friends, coworkers, neighbors, and our community. Studies show that people with more social connections live longer than those who face isolation, loneliness, and poor-quality relationships. In fact, the lack of social connections is as dangerous as smoking up to 15 cigarettes a day or drinking six alcoholic drinks daily, according to the Office of the U.S. Surgeon General.7
Communities can work together to create the conditions that support good mental health and well-being. Instead of leaving people to face these challenges alone, we can use community-wide strategies to improve living conditions and make sure treatment is safe and easy to get when a mental health crisis happens. -
What are the Disparities?
Everyone can experience mental health challenges. However, because community and social conditions impact our mental health, some groups are more at risk for mental distress.
Adults
Tennessee adults can experience many challenges that affect their mental well-being. In 2022, about one in five adults reported frequent mental distress.5 This means their mental health was not good for at least 14 days (about 2 weeks) of the past month. Poverty can contribute to these challenges by increasing stress and limiting access to care and support. In 2023, 14% of Tennessee adults lived in poverty, slightly higher than the national rate of 12.5%.9
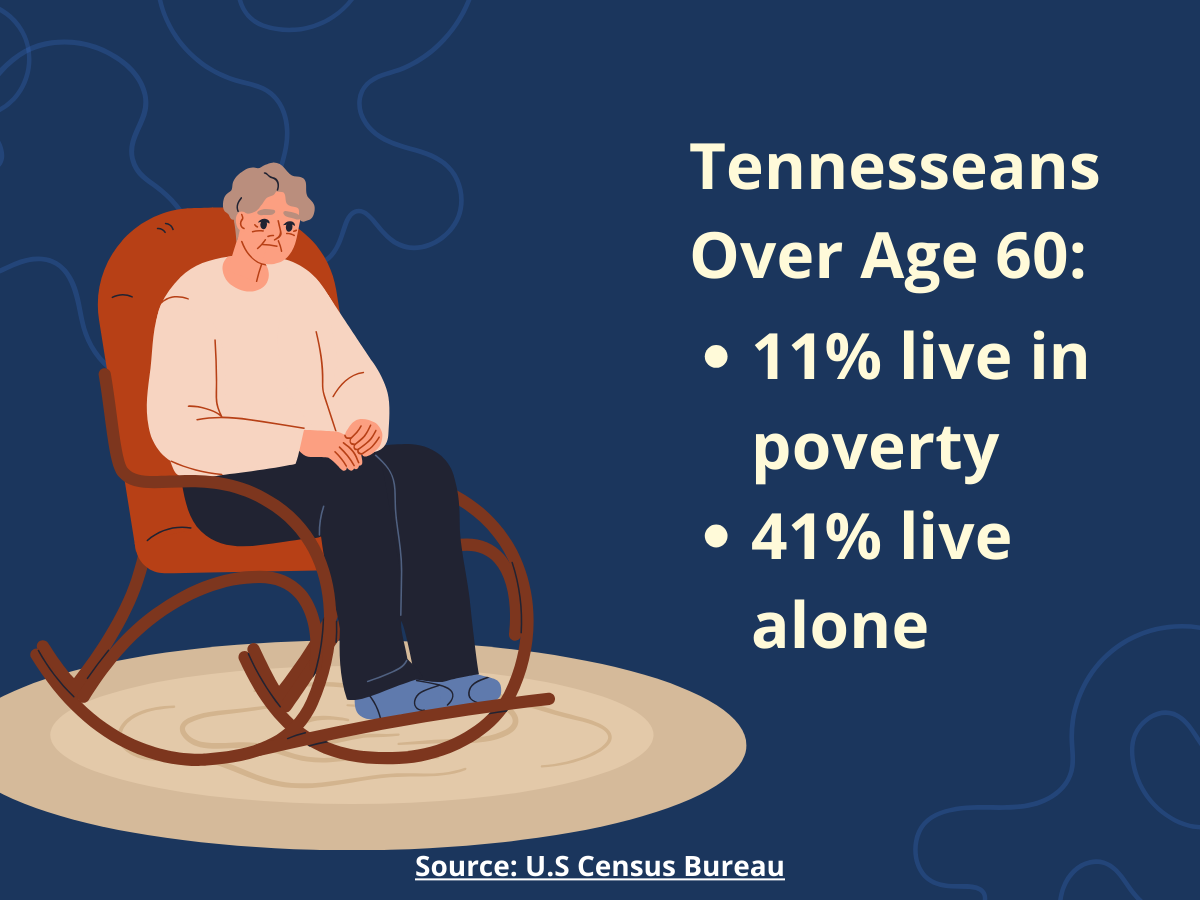
Older Adults
Older adults in Tennessee face many challenges to their mental well-being. Life changes like retirement, serious illness, or losing a loved one can result in grief, loneliness, and social isolation.10 In 2023, 10.8% of older adults in the state lived in poverty, and 11.5% lived alone, increasing risks of stress and social isolation. 9,11
Older adults may also face unique barriers to mental health care. They might think symptoms like depression are a regular part of aging, feel stigma or shame, or not realize treatment could help. Cost, transportation, or a lack of local services can limit access of care.10 Healthcare professionals may overlook symptoms or mistake them for physical illness, or they may not always have the training to screen or treat mental health conditions in older adults.10
With the older adult population expected to grow by 30% by 2040, access to care and support will be increasingly important.5
Children
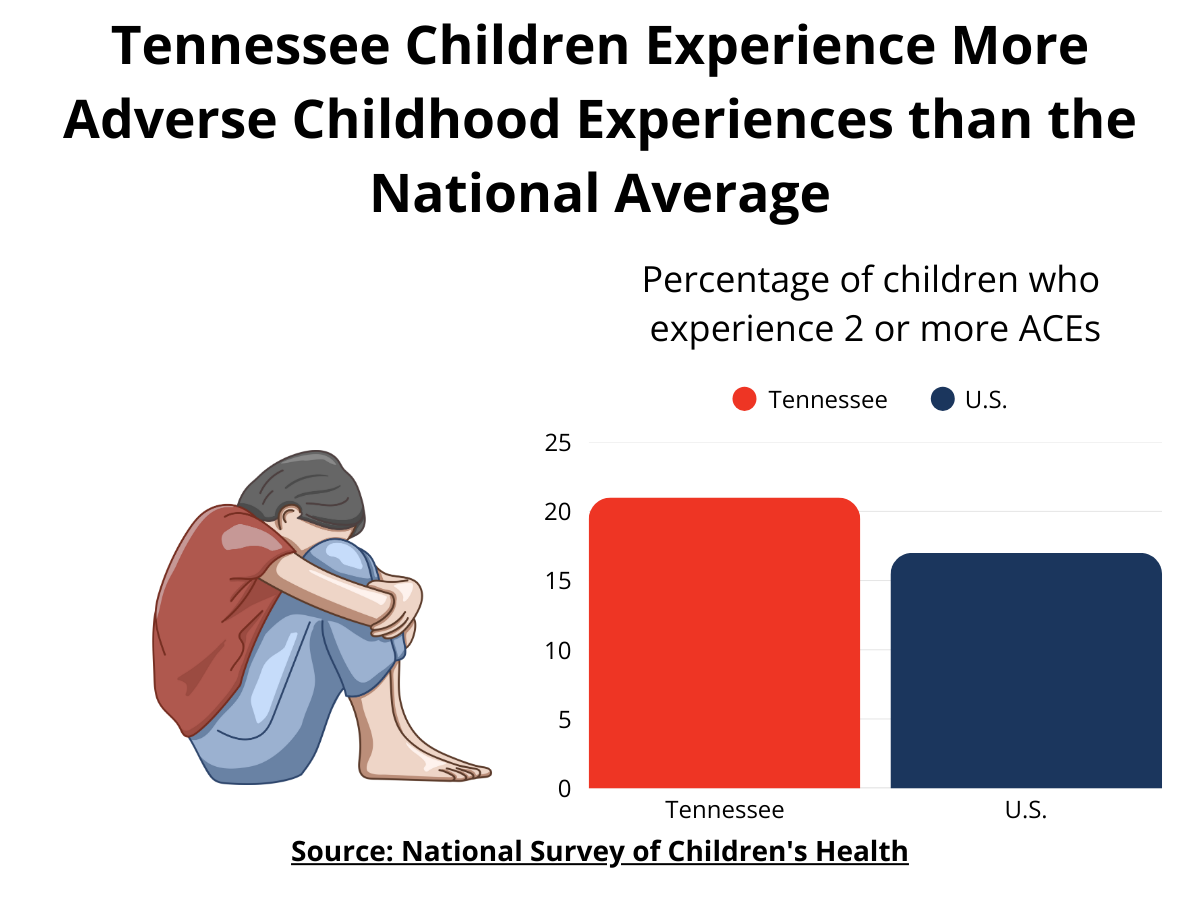
Mental well-being begins at birth. According to the CDC, one in six children ages 2-8 has a diagnosable mental health condition.12 Tennessee ranks 35th in the U.S. for adverse childhood experiences, placing it among the states with the highest rates.13 According to Harvard’s Center on the Developing Child, adverse experiences early in life can impair the foundation for all future learning, behavior, and health.14 Adverse childhood experiences, or ACEs, are potentially traumatic events that occur in childhood.15 Children who have multiple ACEs tend to have more physical and mental health problems later in life.
Youth
About one in five U.S. children ages 12 to 17 may have a mental health or behavioral condition.16 In Tennessee, one in four high school students reports that their mental health is not good most or all of the time.17 Among Tennessee youth with a Major Depressive Episode in 2024, 62.4% percent did not receive any treatment.18
Reasons people gave for not getting treatment include:19
- They thought they could handle it on their own
- They worried about what others would think
- They worried their information would not be kept private
- They did not know how or where to get help
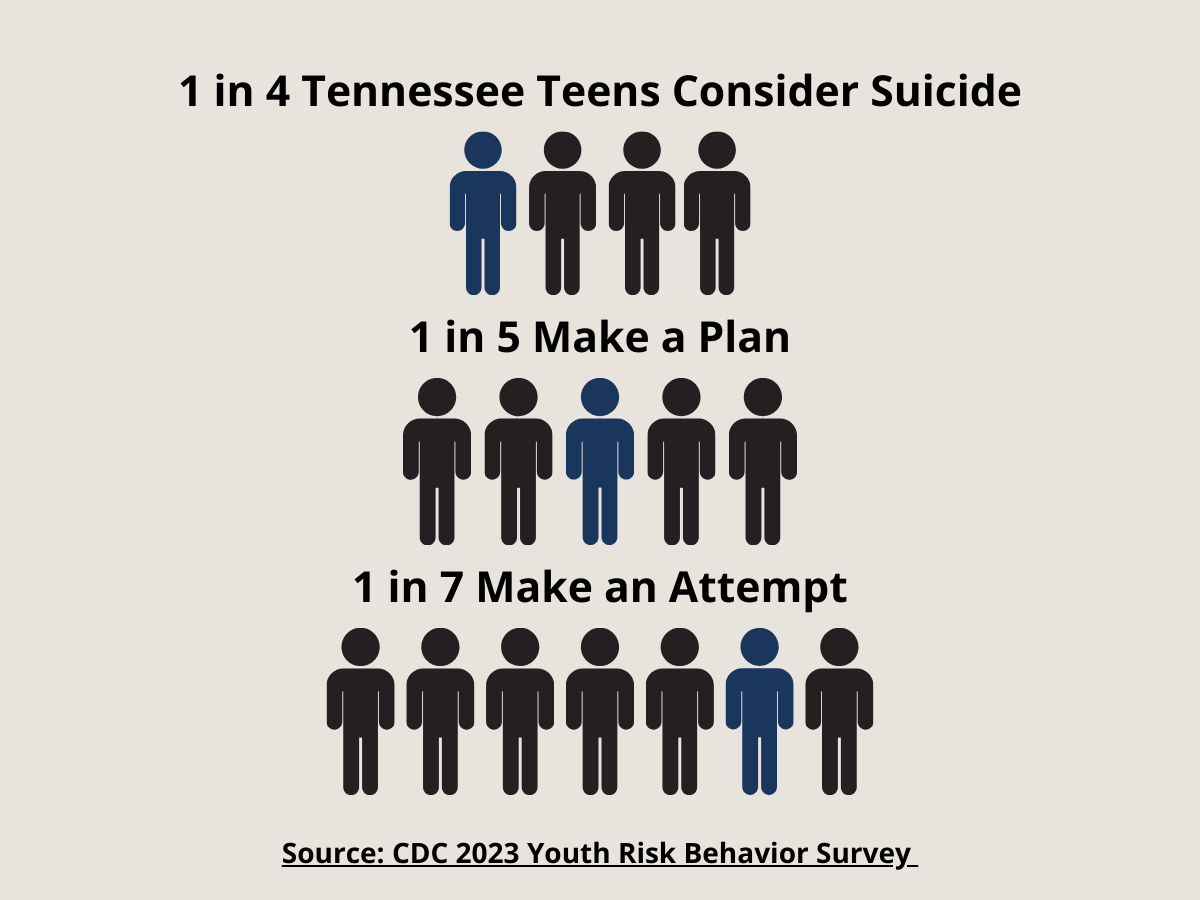
Data from the CDC’s 2023 High School Youth Risk Behavior Survey reveals that many Tennessee teens have considered harming themselves. One in three high school girls and one in seven high school boys reported they tried to lose weight or stop gaining weight by using unhealthy methods.20 These included not eating for a full day, using diet pills or powders, making themselves vomit or taking laxatives, smoking cigarettes, or skipping meals. More than one in four high school students reported that, within the last 12 months, they had intentionally hurt themselves, such as cutting or burning themselves, without wanting to die.20 Nearly one in four reported considering suicide; one in five made a plan; and one in seven actually attempted suicide.21–23 These numbers show the importance of providing students with supportive environments, access to mental health services, and resources to help them cope and thrive.
Incarcerated Individuals
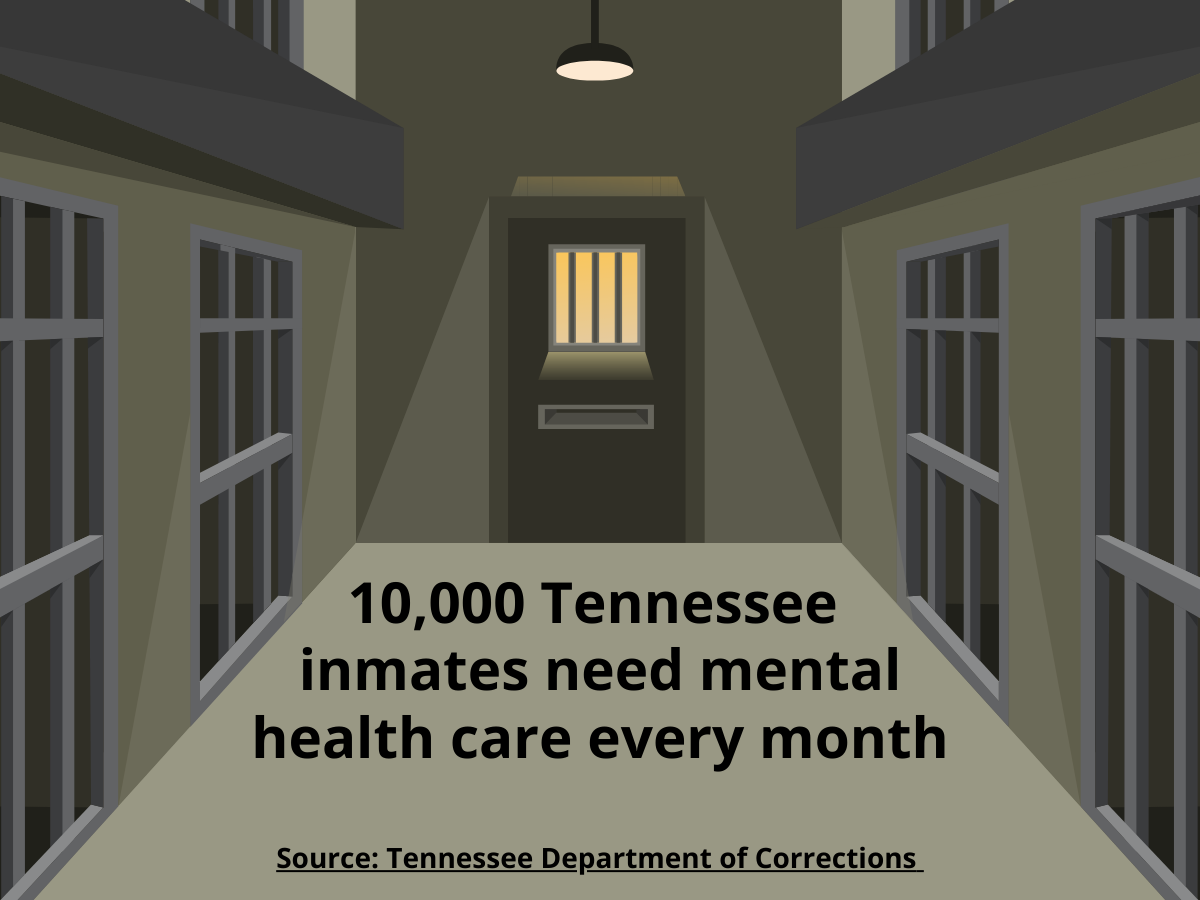
Prisons and jails were not built to be treatment centers, and they lack the funding to give people with serious mental illnesses the complete care they need. As a result of the large, incarcerated population, prisons function as some of the largest providers of mental and physical health care in the United States.24 According to the Substance Abuse and Mental Health Services Administration, around 44% of people in jail and 37% of people in prison have a mental illness.25 Overcrowding, lack of privacy, constant noise, and safety concerns can increase stress and worsen mental health.26 Some former inmates say they often felt like providers dismissed or ignored their mental health complaints, or that they thought the inmates were faking their ailments. However, many physical and mental health needs go unmet in prison, affecting people both while they are incarcerated and when they return to their communities. Receiving quality care during incarceration is critical for managing existing and new conditions, as well as for reducing health risks after re-entry.24
About half of the inmates in Tennessee, or around 10,000 each month, need mental health care.27 According to the Tennessee Department of Corrections, about two-thirds of inmates with a mental health diagnosis have more than one.27 In 2024, TDOC Behavioral Health reported 21,622 total diagnoses, with 11,370 inmates with at least one diagnosis.27
Uninsured/Underinsured Individuals
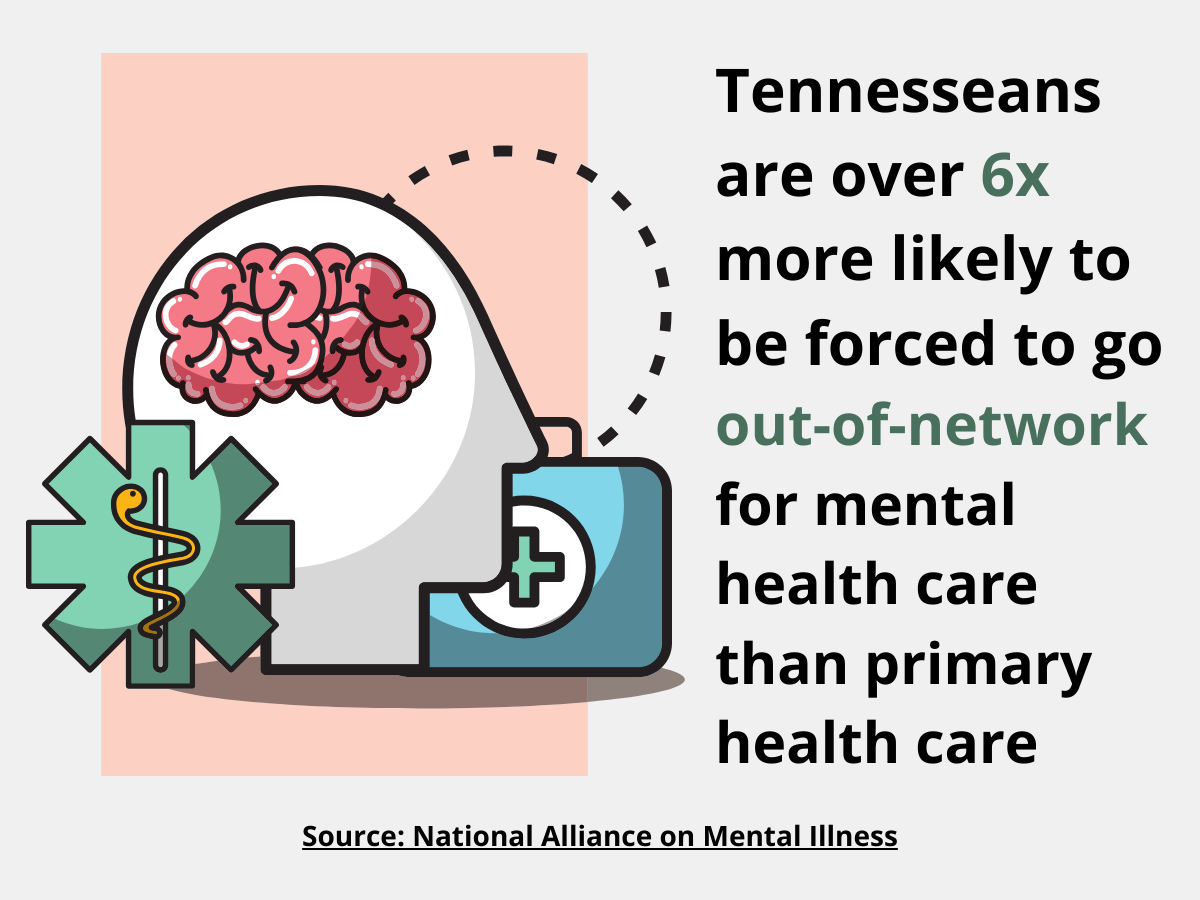
The cost of mental health care is a major barrier to people seeking mental health treatment. The percentage of uninsured adults and children in Tennessee has remained higher than the national average for several years. In 2023, 9.3% of Tennessee adults did not have health insurance, compared to 7.9% nationally.28 Tennesseans with health insurance are twice as likely to be forced to seek treatment out-of-network.29 Because of these insurance gaps, many people in Tennessee struggle to find or afford the mental health care they need.
Unhoused Individuals
Being able to find and keep housing affects a person’s mental health, and having a serious mental illness can also make it harder to get or keep housing. Stress, uncertainty, and threats to safety can increase the risk for mental illness for unhoused people.30 According to the 2024 U.S. Department of Housing and Urban Development Point-In-Time Count, an estimated 8,280 Tennesseans were experiencing homelessness.31 Helping people find stable housing can improve their mental health and lower health care costs.32
LGBTQ+
LGBTQ+ people often face unique challenges that can affect their mental health. Some report being treated unfairly by providers, which can cause fear of discrimination and may make them hesitant to seek care.33 Research shows they are more than 2.5x likely to experience depression or anxiety than their heterosexual peers.33 However, studies also show that they are twice as likely to seek mental health support.34 More than half of LGBTQ+ young people ages 13 to 24 say they have felt symptoms of depression (54%), and two out of three report experiencing anxiety (67%).35 Transgender adults also report higher rates of serious psychological distress than the general population.36 These numbers highlight the importance of creating safe, supportive environments where LGBTQ+ individuals feel valued and can access the care they need to thrive.
Veterans
Active military and veterans are more likely to face mental health problems such as PTSD, depression, or drug and alcohol use.37 This is often because of the stress of military life, combat, and other traumatic experiences. Many veterans say their PTSD symptoms get worse when they leave the military. They may struggle with anger, alcohol or drug use, and problems in their relationships.38 Veterans also die by suicide at a higher rate than non-Veterans.39 Veterans accounted for about 15% of all suicides in Tennessee in 2022.40
-
Community-Driven Solutions
Community-driven solutions are proven steps community groups can take now to support mental well-being and create communities where everyone can do well.
- Create community programs where neighbors can connect and students can establish social skills and generate opportunities for high-risk populations to create a sense of community and build relationships.
- Host community events that bring community members together to socialize and build relationships. This can include game nights, neighborhood BBQs, movie nights, and farmers' markets with local businesses as partners.
- Create or improve community spaces like recreation centers or gyms, providing members of your communities with safe indoor and outdoor places where they can gather, hang out, and hold events.
- Reduce the stigma around mental health by talking openly about mental health, educating your community, and being conscious about the language you use surrounding mental health.
- Host a Mental Health First Aid training to teach community members how to identify and respond to mental health crises. To inquire about hosting a training through the Department of Health, email MHFA.training@tn.gov.
- Increase access to safe green spaces like parks and gardens. Spending more time outdoors in nature has been shown to reduce stress, improve mood, and decrease the risk for developing a mental health condition. Check out the Office of Primary Prevention’s list of funding opportunities.
- Create intergenerational programs that increase connections and support to develop and maintain relationships between youth and older adults. Create programs that unite youth and older adults and foster relationships.
- Improve Insurance and Access. Make sure mental health care is covered in the same way as physical health care. Give workers paid sick leave, flexible schedules, and mental health days. Put rules in place to help protect people from stress and burnout.
-
Making Change through Policy and Systems
- Support policy initiatives that address the root causes of desired mental health goals. Conduct a root cause analysis to explore factors contributing to mental health challenges for your community. Conducting a root cause analysis will allow you to identify and tackle the underlying causes surrounding mental health and help you to strengthen your community.
- Get involved with a Regional Policy and Planning Council. These groups include mental health and substance abuse service providers, consumers, family members, advocates, and other stakeholders who advise the Tennessee Department of Mental Health and Substance Abuse Services about the service system, policy development, legislation, budget requests, system evaluation, and monitoring.
- Influence policy and legislation by exploring opportunities to incorporate community prevention strategies into already-existing mental health policies and regulations.
- Encourage community institutions such as healthcare, education, housing & development, and business, to include community mental health to prioritize community mental well-being in activities such as hiring, purchasing, and workplace policy development.
- Engage community leaders in collaborations with multiple sectors (including health, education, criminal justice, law enforcement, business, housing, and more) to explore strategies that advance community well-being.
- Bring together mental and behavioral health practitioners to discuss implications and opportunities to advance community prevention that complements treatment and early intervention strategies.
-
Community Spotlight
The Health Council Community of Practice (CoP) connects Tennessee Health Councils through shared learning and discussion around health priorities. The links below provide access to recent CoP conversations related to this topic. To learn more about the Community of Practice, click here.
Trousdale County (January 2024)
Hickman County (November 2024)
NAMI Davidson (April 2025)
Lincoln County (May 2025)
Robertson County (December 2025)Submit your own Community Spotlight! Please email Health.Councils@tn.gov with any relevant stories, resources, or presentations related to this topic.
-
Partners and Resources
Statewide Resources
Tennessee Department of Mental Health & Substance Abuse Services:
- Behavioral Health Safety Net (BHSN)
Services are available for anyone 3 years of age or older who has a qualifying mental health diagnosis and does not have behavioral health insurance. This program provides assessment, evaluation, diagnostic, therapeutic intervention, case management, transportation, peer support services, psychosocial rehabilitation services, psychiatric medication management, labs related to medication management, pharmacy assistance, and coordination. - “Be the One” Suicide Prevention Campaign
"Be the One" is a training that equips staff members with the tools and resources necessary to recognize when someone they know may be thinking about suicide. It teaches how to ask questions directly and offers tips on developing good listening skills, a key component of suicide prevention. Training also provides individuals with the tools necessary to instill hope when someone you know seems to have lost all hope. - Crisis Intervention Teams (CIT)
These teams improve the outcomes for people living with mental health challenges who encounter law enforcement. CIT training is a specialized 40-hour program for law enforcement officers to improve outcomes of encounters with people living with behavioral health challenges. - Crisis Services for Children and Youth
These services are provided by Youth Villages, Mental Health Cooperative, Frontier Health, and the McNabb Center across Tennessee. Emergency counselors (triage specialists) handle calls 24/7 through their regional hotline and determine an appropriate response. You can access mobile crisis services by calling or texting 988 and pressing 0 to speak with a crisis counselor. - TN Voices
TN Voices is a statewide leader in mental health and family well-being, providing free therapy for pregnant moms across Tennessee. Therapists provide a safe and private space to talk through the emotional challenges of pregnancy and beyond, offering support every step of the way. - Crisis Services Map
This TN Department of Mental Health & Substance Abuse Services map shows crisis services and providers across the state. -
Crisis Stabilization Units (CSU)
CSUs offer 24/7/365 intensive, short-term stabilization for someone who is experiencing a mental health emergency and is willing to receive services. The average CSU stay length is three days, and the service is free of charge. -
Crisis Walk-in Centers
These centers offer face-to-face, 24/7/365 evaluation for those who are experiencing a mental health emergency. To find a walk-in center closest to you, call 855-CRISIS-1 (855-274-7471). -
Hospital Services
The Tennessee Department of Mental Health & Substance Abuse Services operates four Regional Mental Health Institutes (RMHIs) in Bolivar, Chattanooga, Memphis, and Nashville. All RMHIs are accredited by The Joint Commission and have deemed status with the Centers for Medicare and Medicaid Services. The program also contracts with three privately-run psychiatric hospitals in East Tennessee for involuntary admissions to inpatient psychiatric treatment. -
Map of Statewide Crisis Services
This link provides a map of mobile crisis teams, crisis stabilization and walk-in clinics, regional mental health institutes, respite services, and medically monitored withdrawal management. -
Mobile Crisis Services
MCS is a 24/7 response team for those who are experiencing a mental health emergency. -
On Track TN: First Episode Psychosis Initiative
This initiative is designed to provide early intervention for youth and young adults between the ages of 15 and 30 who have experienced first-episode psychosis. This comprehensive intervention model involves a team of mental health professionals and support services, focusing on helping people work toward recovery and meeting personal goals. -
Project B.A.S.I.C. (Better Attitudes and Skills in Children)
This project is a school-based program that helps kindergarten through third-grade students build strong mental health. The program includes identifying children with serious emotional challenges, consultations with teachers and students, creating a positive school environment, and classroom mental health lessons. The Project Basic Helpline, 800-560-5767, is available Monday-Friday from 8:00 to 4:30 pm, or email: OCA.TDMHSAS@tn.org. -
Suicide Prevention Programs
These programs offer a variety of services that provide prevention and postvention for those who are experiencing suicidal thoughts or a post suicidal crisis, including family support to those who have completed suicide. -
TN Statewide Crisis Hotline
This hotline is free and available 24 hours a day, 365 days a year. It is a resource for anyone who is experiencing a mental health crisis. A trained crisis counselor in your area will answer and provide you with support, guidance, and work to connect you with appropriate community support.
Other Tennessee Resources
- Mental Health Cooperative (MHC)
MHC offers behavioral health services for children, adolescents, and adults that address the specialized needs of people with several behavioral health conditions and poverty-related challenges. MHC has 12 locations across Middle Tennessee, Chattanooga, and Memphis. MHC accepts all TennCare plans, and grants are available for the uninsured. - National Alliance on Mental Illness (NAMI)
NAMI can help you locate support groups or other mental health services around the state on namitn.org. A toll-free resource helpline, 800-467-3589, is available Monday-Friday, 9:00 am to 5:00 pm CST. - The Tennessee Association of Mental Health Organizations (TAMHO)
TAMHO is a statewide trade association representing Community Mental Health Centers and other nonprofit corporations that provide behavioral health services. The TAMHO website provides a county-by-county directory of mental health service providers. Help is also available toll-free at 800-568-2642. - TN Voices
This service promotes the use of a coordinated system of care in Tennessee that includes family support and community engagement as key components. TN Voices works collaboratively to ensure that the services provided to children and families in Tennessee are family-driven, community-based, and culturally and linguistically competent. - Tennessee Suicide Prevention Network (TSPN)
TSPN is a statewide organization that works to reduce the stigma of suicide and support prevention efforts across Tennessee. TSPN organizes regional groups that meet regularly to share resources and ideas for local communities. The organization also provides brochures with helpful information and promotes the statewide crisis hotline: 855-CRISIS-1 (855-274-7471).
To Learn More
988 Suicide & Crisis Lifeline is a free phone number anyone in the U.S. can call or text if they are feeling sad, hopeless, worried, or thinking about suicide. When someone calls, trained counselors listen, give support, and help the person feel calmer and safer. They can also connect callers to local resources, like mental health services, if more help is needed.
Rural Health Information Hub
Mental Health in Rural Communities Toolkit
This toolkit compiles evidence-based and promising models and resources to support organizations implementing mental health programs in rural communities with a primary focus on adult mental health.Substance Abuse and Mental Health Services Administration (SAMHSA)
Community Conversation about Mental Health: Information Brief Toolkit
This toolkit is designed to help individuals and organizations who want to organize community conversations achieve three potential objectives: get others talking about mental health to break down misperceptions and promote recovery and healthy communities; find innovative community-based solutions to mental health needs, with a focus on helping young people; and develop clear steps for communities to address their mental health needs in a way that complements existing local activities.US Department of Veterans Affairs
Veterans Crisis Hotline
This hotline is a 24/7 confidential crisis support for veterans and their loved ones. You do not have to be enrolled in VA benefits or healthcare to call. - Behavioral Health Safety Net (BHSN)
 Stout Drive Road Closure
Stout Drive Road Closure