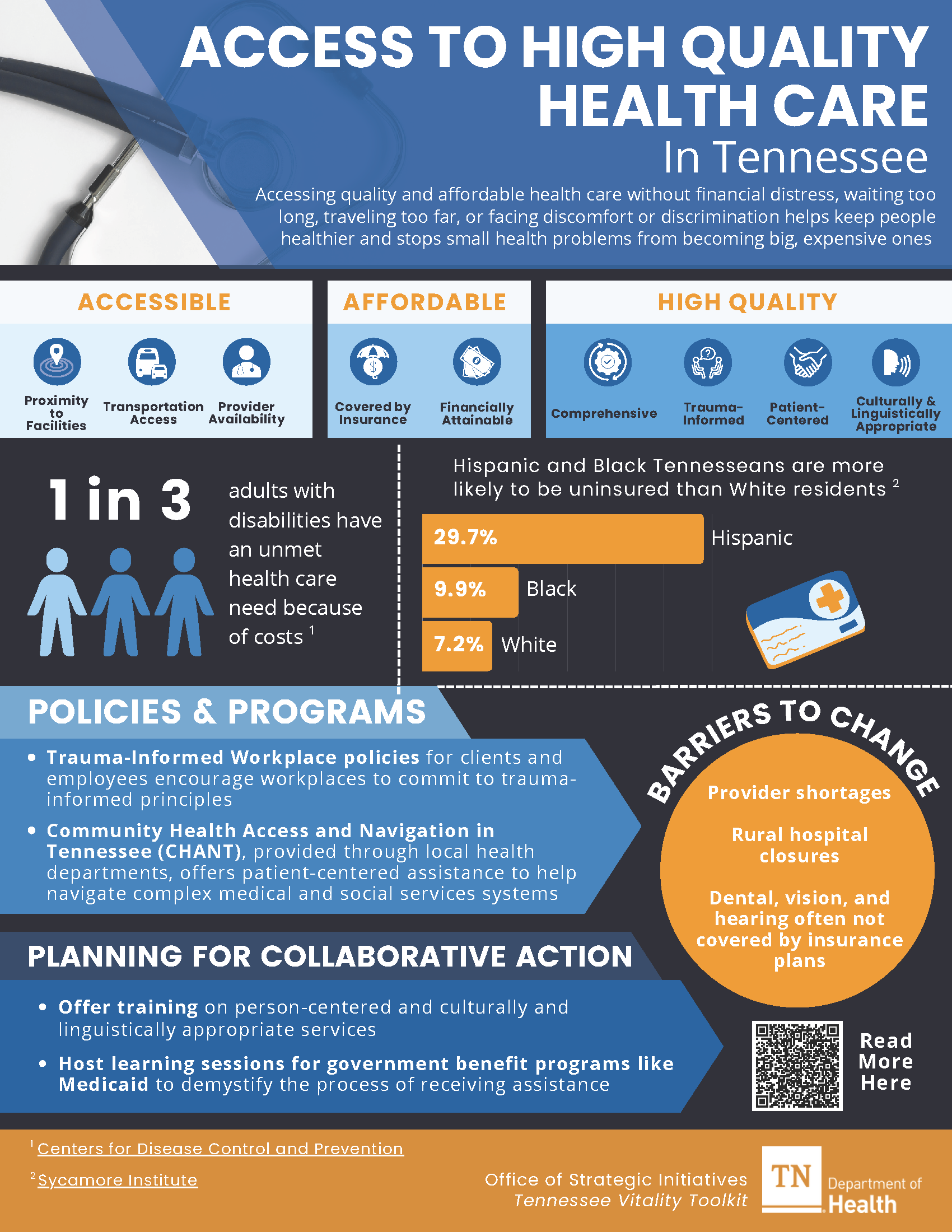
Access to High Quality Health Care
Getting quality, affordable health care means people can see a doctor when needed—without spending too much, waiting long, traveling far, or feeling uncomfortable or mistreated. This helps people stay healthy and keeps minor problems from becoming serious. When health care is easy to reach and affordable, people are more likely to get regular checkups, manage ongoing conditions, and get help early when something feels wrong.1
Many people in the United States do not get the health care that they need.2 This can be even more challenging in Tennessee because there is a shortage of doctors, dentists, and mental health providers.3–5 This means many people struggle to find care close to home when they need it.
What Makes Health Care Accessible?
Several factors determine whether people can get the care they need when they need it:
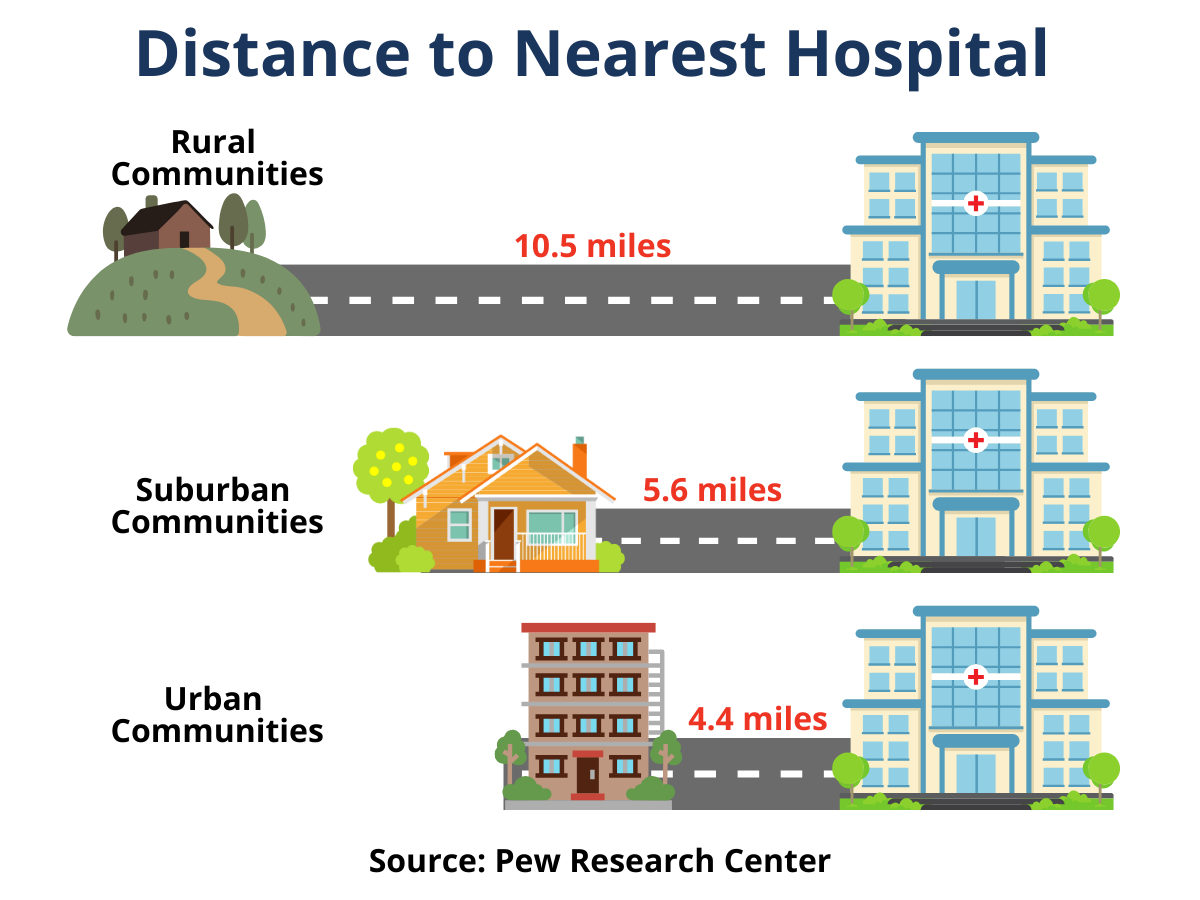
- Proximity: Are clinics and hospitals close to where people live? 6
- Transportation: Do people have a reliable way to get to and from appointments? Are clinics easy to reach by public transportation? 7
- Provider availability: Are there enough doctors, dentists, and other health care professionals to meet the community’s needs? Can people get appointments without long waits? 1,2
- Affordability: Can people pay for visits, medicine, and follow-up care without financial strain? Does the provider offer sliding scale services or financial assistance? 8
- Health insurance: Do people have insurance that helps cover the cost of care? Are they able to find providers who accept their coverage? 9
- Language and communication: Can people easily understand their health care providers, and can providers communicate clearly in languages patients speak? 10
- Comfort and trust: Do people feel welcomed and respected when they seek care, without fear of discrimination or judgment? 11
Access is only part of the story—high-quality care is also essential. Even if people can easily access care, it must meet their needs, treat them with respect, and support both their physical and mental health. When care is high quality, people are more likely to get the help they need, feel safe and valued, and stay healthier overall.
What Makes Health Care High-Quality?
Several factors determine whether people are getting care that truly meets their needs:
- Comprehensive: Can people get a range of services—both mental and physical health care—in one place? 12
- Trauma-informed: Do people feel safe, comfortable, and respected when they receive care? 13
- Patient-centered: Do providers listen, involve patients in decisions, and treat them as people, not just as medical problems? 13
- Respectful of different cultures and languages: Can providers meet the language and cultural needs of the people they serve? 14
Together, accessible, high-quality health care helps people get the right care at the right time, in a way that works for them and keeps communities healthier overall.
-
Why is Access to High-Quality Healthcare Important for Community Well-Being?
Access to affordable, high-quality care helps communities stay healthier overall. But good health care is more than just treating sickness. It’s also about preventing disease and improving the social and community conditions that affect health. This includes helping people stay healthy through regular care, early treatment, and connections to community support.
Preventing disease and supporting health often depends on more than health care services alone. The social determinants of health (SDOH) are the everyday conditions in which people are born, live, work, and grow older.15 These conditions affect how easy or hard it is to stay healthy and can lead to differences in health between groups of people.16 Because these conditions are not the same for everyone, some groups face more obstacles to good health and often have worse health outcomes than others.

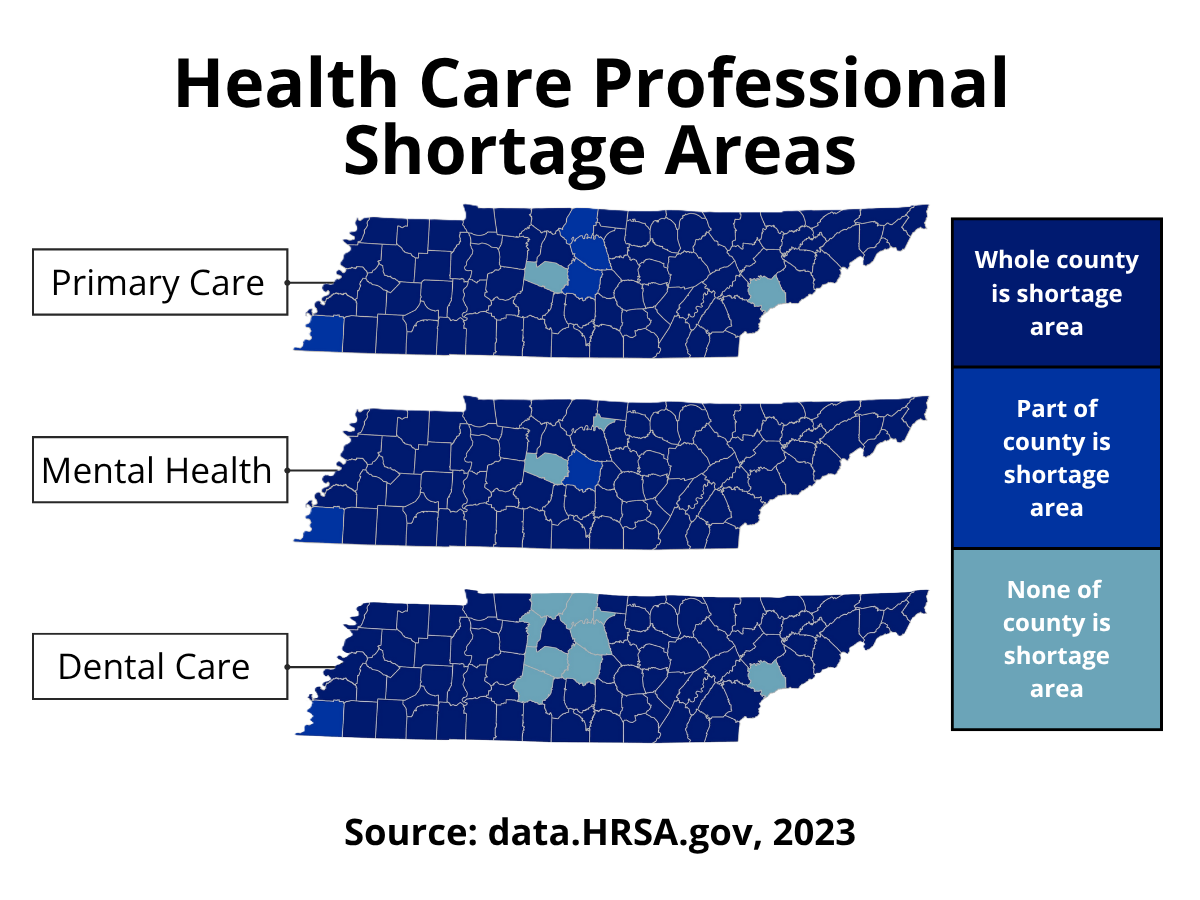
In Tennessee, many factors—such as low income, lack of transportation, unstable housing, and difficulty understanding health information—can make it hard for people to get regular medical care.17 These barriers can prevent people from finding a primary care doctor or keeping up with routine check-ups. Another major challenge is the state’s shortage of primary care doctors, dentists, and mental health providers. According to HRSA data, all but two of Tennessee’s 95 counties are considered Primary Care and Mental Health Professional Shortage Areas, and only nine counties have enough dentists to meet their populations' needs.3–5
According to the CDC, in 2023, 17% of Tennesseans lacked a personal health care provider.18 People with a trusted provider are more likely to get preventive care such as vaccines, screenings, and check-ups. They also tend to seek care sooner when a health issue arises.
Strong health care depends not only on medical treatment but also on the support and conditions that help people stay healthy every day. Hospitals and health organizations in Tennessee can also play a key role. They can work with County Health Councils to connect their required Community Health Needs Assessment (CHNA) with local health improvement plans. This teamwork helps hospitals and communities work toward the same goals—addressing the social factors influencing health and building stronger, healthier communities.
When people in Tennessee have access to quality and affordable health care, they are healthier, can work more effectively, and help their communities grow stronger over time.
-
What are the Disparities?
Some groups in Tennessee have a harder time getting high-quality health care. This includes people without insurance, those living in rural areas, older adults, people with disabilities, racial and ethnic minorities, and people with limited English skills.19,20 These challenges can keep people from getting the care they need, leading to poorer health.
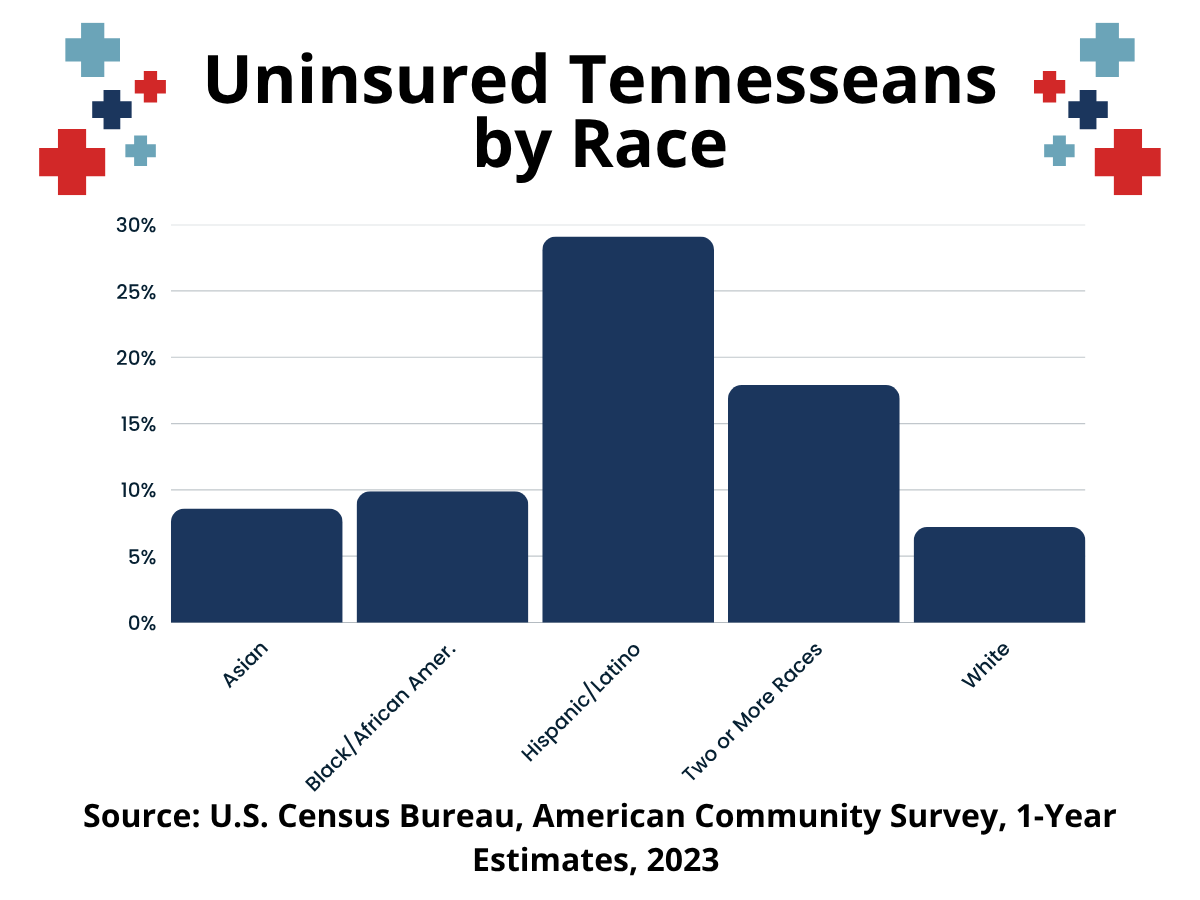
Uninsured Tennesseeans
Having health insurance is an essential step toward getting routine, high-quality care. In Tennessee, some communities have higher rates of uninsured residents than others. When people don’t have coverage, the cost of care often keeps them from seeing a doctor when they need to. Recent data showed that 13% of Tennessee adults in 2023 could not see a doctor due to cost, highlighting the ongoing financial barriers to care across the state.21
Being uninsured can lead to worse health outcomes for both adults and children. For example, uninsured pregnant women are less likely to have early prenatal checkups, which can affect the health of both the mother and baby.22 Uninsured Tennesseans also have lower HPV vaccination rates, increasing their risk for certain cancers.23 Children with mental health conditions like anxiety or depression who have no or limited insurance are also more likely to face barriers to getting mental health care.24Health coverage for children is essential for their growth and development. In Tennessee, about 6.8% of children ages 6–18 and 6.1% of children under 6 are uninsured.25 Many of these children are eligible for coverage through the CoverKids program, but their families may not know about it or how to apply. This shows how health literacy barriers, such as trouble finding, understanding, or using health information, can keep families from getting the coverage their children need.
Expanding awareness of insurance options and simplifying the enrollment process for programs like CoverKids can help close the gap. When more Tennesseans have health insurance, they can get preventive care, manage health issues early, and build a foundation for better health across all stages of life.
Children
Every child deserves a healthy start in life, but many Tennessee children face challenges getting the care they need. Access to affordable, consistent, high-quality health care helps children stay healthy, learn better, and grow into thriving adults.
Many children in Tennessee face barriers to getting the care they need. According to the 2023 National Survey of Children’s Health, about 8.8% of children lived in families that couldn’t pay medical bills in the past year, and 26.7% had no personal doctor or nurse for regular care.26,27 The 2024 State of the Child in Tennessee report also found that the state did not meet any of the Healthy People 2030 goals for 24-month vaccinations, showing gaps in preventive care for young children.28
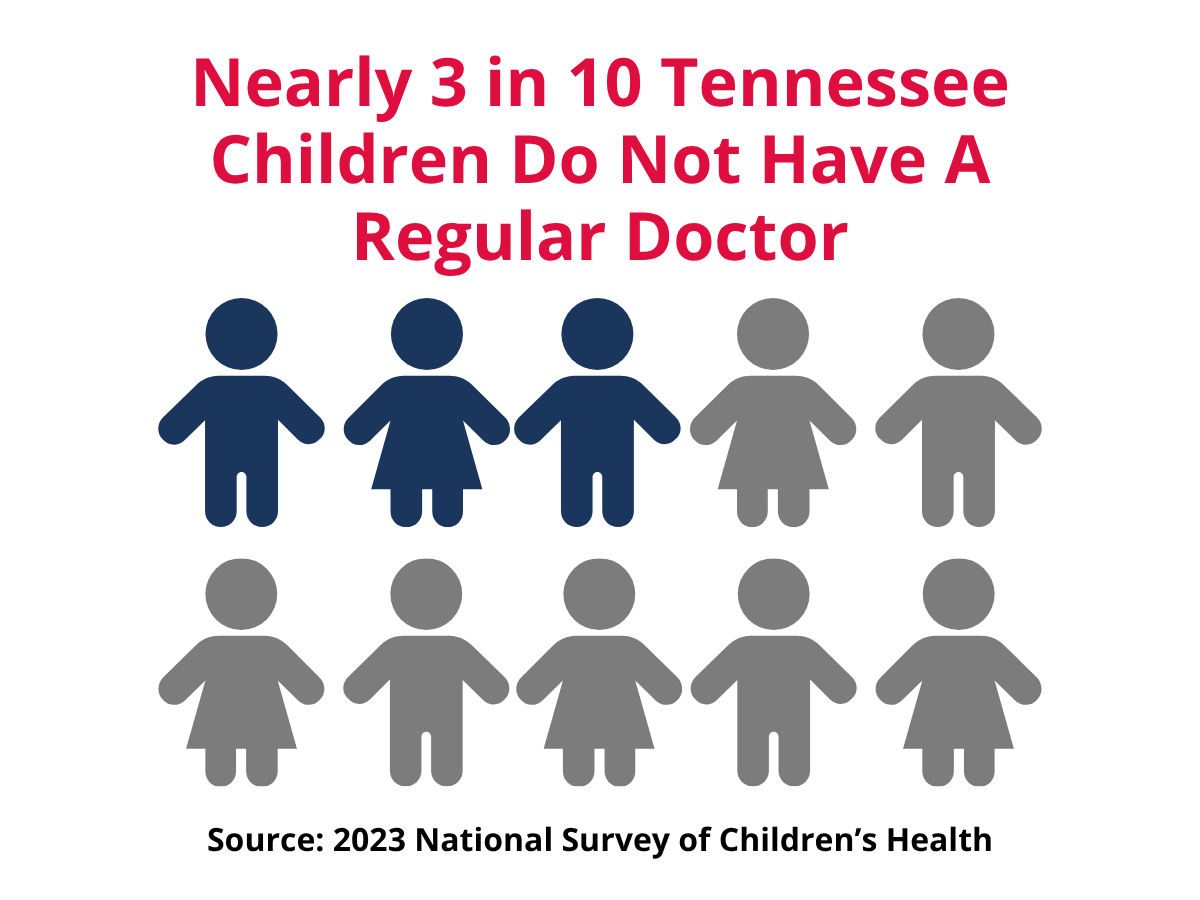
These barriers can affect children’s health now and in the future. Adverse Childhood Experiences (ACEs)—such as abuse, neglect, or family instability—are linked to chronic diseases later in life and higher health care costs.29 This highlights the importance of trauma-informed care that supports children’s mental and emotional well-being.
However, mental health services are not always easy to find. Many Tennessee children, especially those in rural areas, struggle to access mental health care.30 A national study found that about half of children with depression or anxiety face barriers to getting help.24 In 2023, nearly 47% of Tennessee children (ages 3–17) also had difficulty accessing mental health care.31 Since the COVID-19 pandemic, children’s mental health has declined, making these gaps even more serious.32
Children from racial and ethnic minority groups often face additional barriers to care. A statewide study from 2018–2020 found that infants born to Black or Hispanic mothers who were exposed to the hepatitis virus before birth were less likely to receive recommended hepatitis C testing.33 These disparities show the need for health systems to ensure all children—regardless of race, income, or location—can access high-quality care.
Improving children’s access to quality care helps build a stronger, healthier Tennessee. When every child has the chance to receive regular, affordable care—both physical and mental—they are more likely to stay healthy, succeed in school, and contribute to their communities' well-being.
Older Adults
Older adults often struggle to get the health care they need. Many are retired and live on fixed incomes, so high medical and dental costs can strain their budgets. They also report experiencing discrimination in health care, saying they are sometimes mistreated because of their age.34
These financial and social barriers already affect how often older adults seek care. A statewide study found dental visits among Tennessee seniors dropped from 76.5% in 2010 to 71.2% in 2018, showing that cost is becoming a bigger obstacle.35 At the same time, older adults are also more likely to have age-related health problems, like vision or eye diseases, yet many struggle to find providers or get appointments. 36
Cultural or faith-based beliefs can also affect how older adults seek health care. Many older Tennesseans may rely on their faith to cope with stress, make health decisions, and manage illness. For some, prayer and personal spiritual practices help them feel calmer, less worried, and more in control of their health. 37 Others may want health care providers to understand and respect their spiritual needs when talking about treatment or difficult health decisions. 37 Because these beliefs are so important, health services that are respectful, culturally aware, and open to discussing faith can help older adults feel more comfortable getting care and may reduce health gaps. 38
Individuals with Disabilities
Adults with disabilities face some of the highest barriers to accessing high-quality health care. In Tennessee, 33.4% of adults ages 18 and older reported having a disability in 2022, including cognitive (17.1%), mobility (15.6%), visual (7.1%), and hearing disabilities (6.7%).39
Despite their greater health needs, many adults with disabilities struggle to access even basic care. One in four U.S. adults ages 18 to 44 with disabilities does not have a regular health care provider, and another one in four could not afford needed care in the past year. Among adults ages 45 to 64 with disabilities, one in six did not receive a routine check-up.40
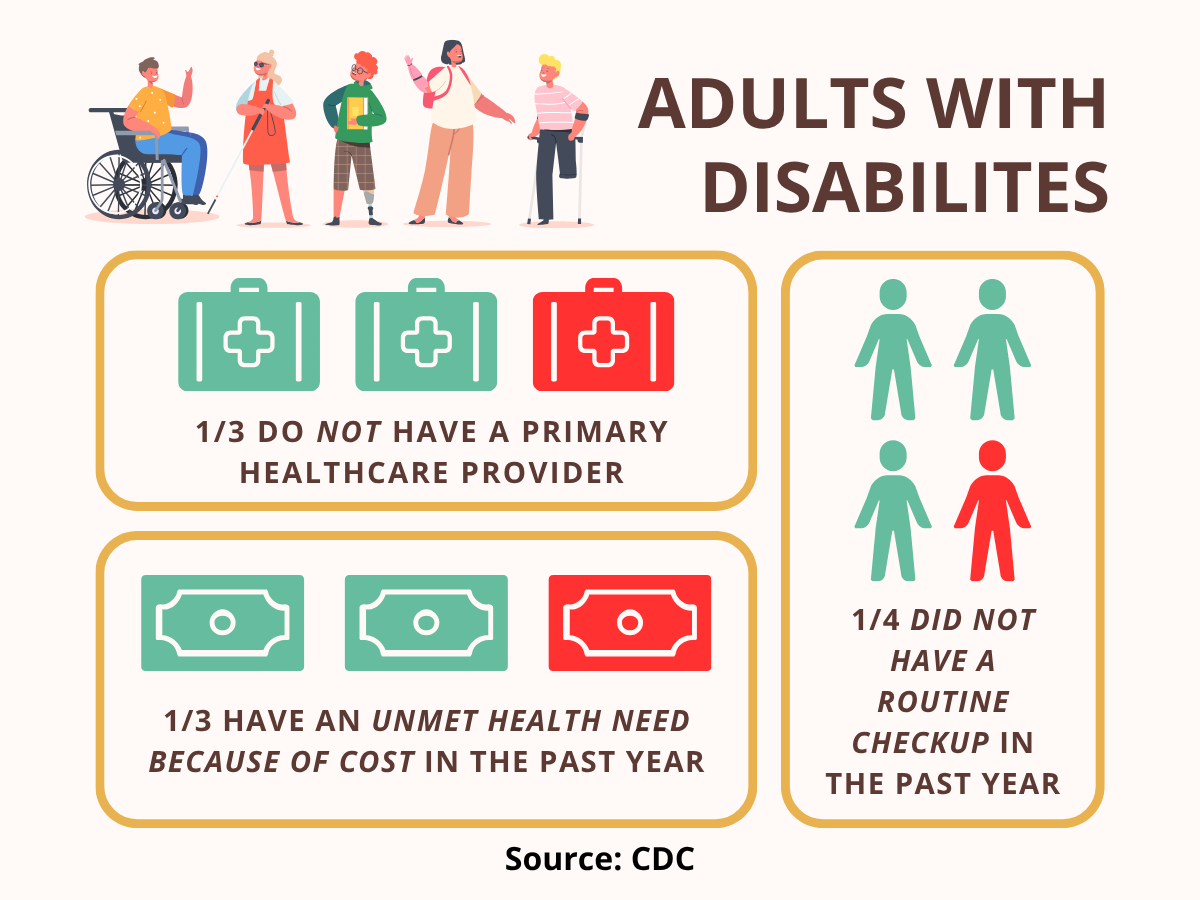
These access barriers lead to worse health outcomes over time. Adults with disabilities have higher rates of chronic diseases than those without disabilities, including obesity (40.5% vs. 30.3%), heart disease (10.4% vs. 3.7%), and diabetes (16.6% vs. 7.9%).40
Improving access for adults with disabilities requires more than the availability of services — care must be affordable, physically accessible, and responsive to different needs. Community outreach health programs have been shown to successfully reach adults with disabilities often missed by traditional health systems.19,41
Low Socioeconomic Status
People with low incomes in Tennessee face significant health challenges that are closely linked to poverty. A study of all 95 Tennessee counties found that higher poverty rates were associated with worse health outcomes, underscoring the extent to which social and economic conditions affect health.42 Another statewide study found that counties with lower median household incomes had higher rates of both overall deaths and deaths from conditions that could have been treated with timely care.43
Health insurance is one of the most significant barriers. People with low socioeconomic status are more likely to be uninsured or underinsured. In 2023, nearly one in five Tennessee adults ages 25 and older with household incomes below $25,000 said they needed to see a doctor in the past year but could not afford to go.44 This leads many to delay care until conditions worsen.
Low-income adults often face multiple overlapping barriers, such as:- Lack of health insurance or limited coverage
- High out-of-pocket costs for visits, prescriptions, or screenings
- Transportation challenges or long travel distances to providers
- Difficulty taking time off work for appointments
- Caregiving responsibilities or family demands 45

These access issues also affect preventive care. Women from low-income families are less likely to receive breast cancer screening services.46 Even when appointments are made, many are missed due to transportation problems, job conflicts, or other personal and family challenges.47
Unhoused Individuals
People experiencing homelessness face many health challenges. They are more likely to develop both infectious and non-infectious diseases due to barriers in accessing health care and social services.48,49 Homelessness and poor health are closely linked: having one increases the risk of the other.49
In 2024, 6,836 Tennesseans experienced homelessness.50 Between 2017 and 2021, 13.3% of Tennessee households faced severe housing problems.51
Adults experiencing homelessness face multiple barriers to high-quality health care, including:
- Lack of health insurance or limited coverage
- Difficulty accessing clinics or providers due to transportation or location
- Inability to maintain regular appointments due to unstable housing
- Lack of identification or medical records
- Stigma or negative experiences when seeking care 53
- Meeting the health needs of people experiencing homelessness requires collaboration between institutions and communities. Programs like these help ensure children experiencing homelessness are enrolled in Medicaid.54
- Community outreach programs and Health Care for the Homeless clinics (part of HRSA-funded health centers) provide vaccines and other health services to unhoused individuals.41,52
Racial and Ethnic Minorities
Racial and ethnic minorities often face discrimination and unequal treatment in the health care system. These experiences can lead to distrust and avoidance of medical services. In a recent study by the Pew Research Center, 55% of Black Americans reported at least one substantial negative experience in health care, and 49% said they believe the quality of the care they receive results in poorer health in their communities.55
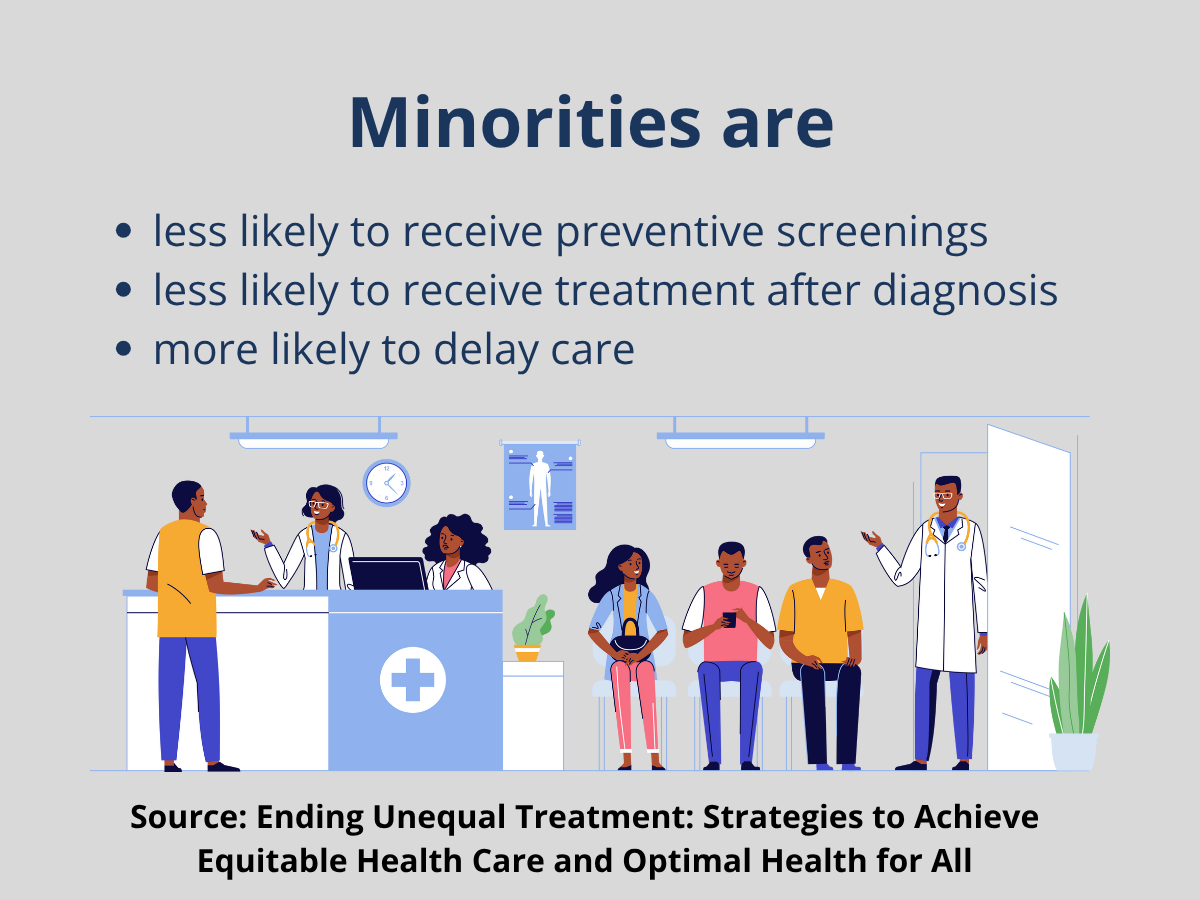
Minorities are less likely to receive preventive screenings, less likely to receive treatment after diagnosis, and more likely to delay care.46,56
For example:
- Black Tennesseans have lower odds of receiving lung cancer treatment compared to White patients.57,58
- Black Tennesseans are more likely to delay prostate cancer treatment.59
- African American patients have higher no-show rates for medical appointments.47
- Black Americans are more likely to express vaccine hesitancy compared to White Americans.60
- Hispanic Tennesseans have higher odds of delayed HIV diagnosis.61
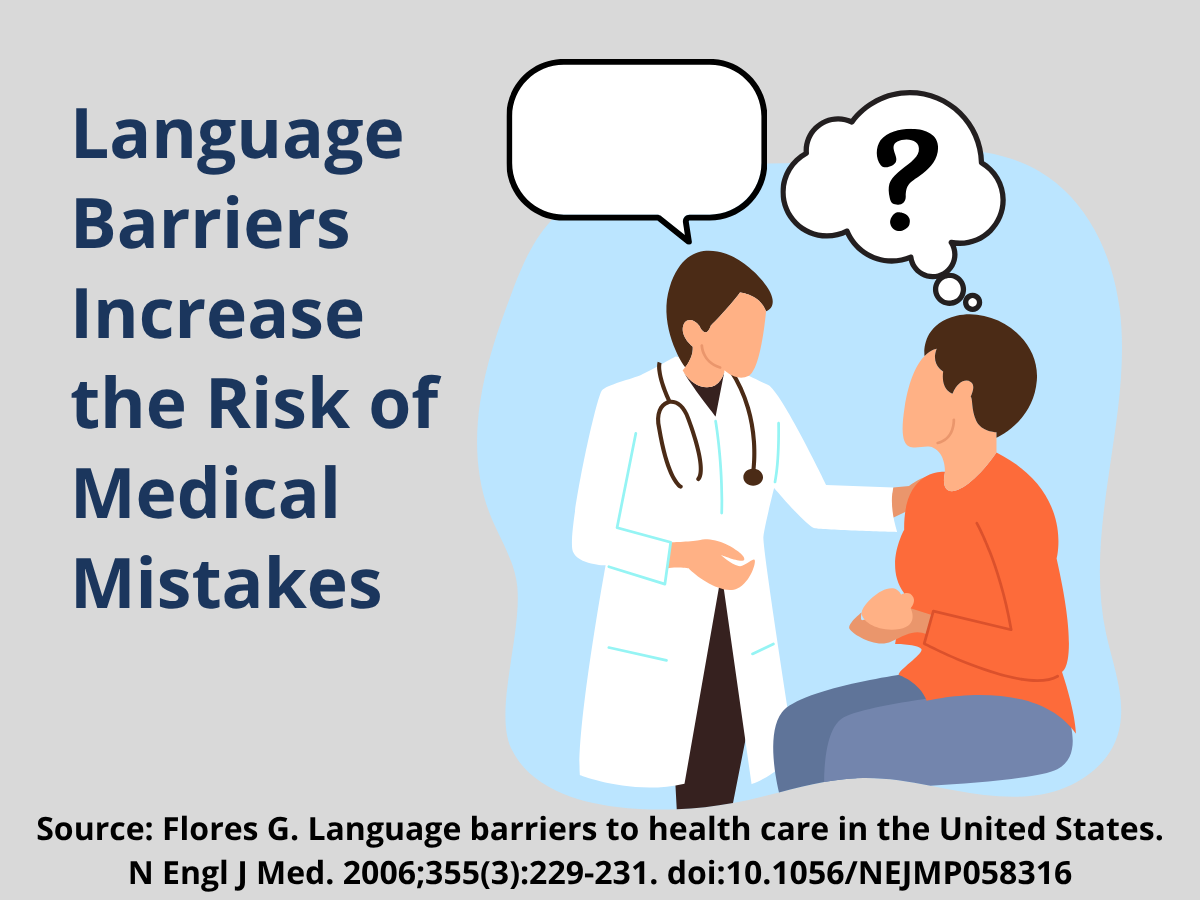
Language access is another significant barrier. Patients with limited English skills often report confusion about medications, difficulty understanding their diagnosis, and higher stress during health care visits.62 When health providers and patients do not speak the same language, it increases the chance of medical mistakes, such as getting the wrong instructions or taking medicine incorrectly.63 People with limited English proficiency are also less likely to get preventive care, such as cancer screenings or vaccines.64
A study in 20 Tennessee counties found that the introduction of new pneumococcal vaccines helped reduce racial disparities in the number of children with invasive pneumococcal disease.65 This improvement shows how expanding access to new medical treatments across all communities can help close long-standing health disparities. Continued investment in similar efforts could further reduce preventable illness among racial and ethnic minority groups.
Rural Communities
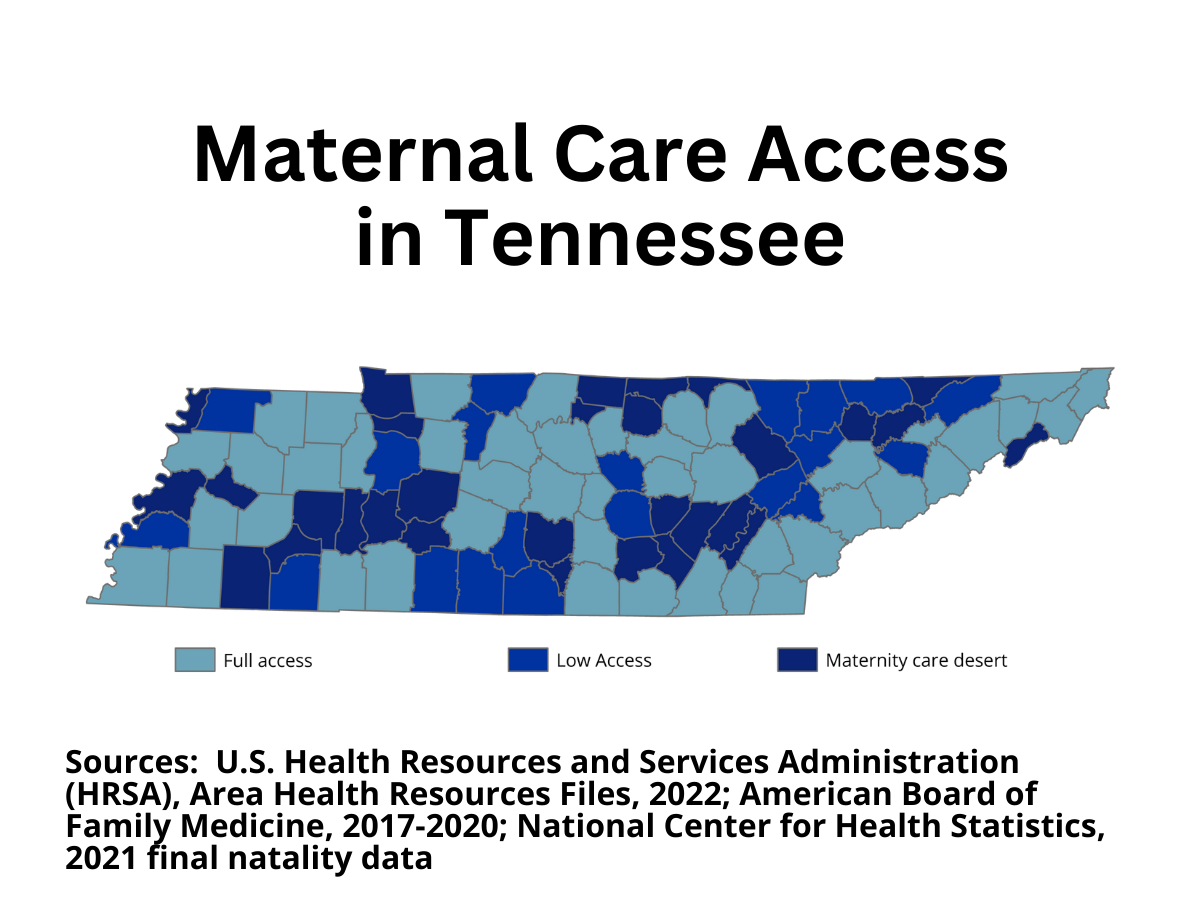
Many people in rural Tennessee struggle to access basic health services. Nearly all rural counties lack enough health providers—98.7% have shortages of primary care and mental health professionals, and 93.5% lack enough dental providers.3–5 Maternity care is also scarce: 32.6% of Tennessee counties are considered maternity care deserts, meaning they have no birthing hospital or maternity provider.66 As a result, 3.4% of women live over an hour from the nearest birthing hospital, and 27% must drive at least 30 minutes for care.66
Hospital closures add to the strain. Since 2010, 15 rural Tennessee hospitals have shut down, primarily due to ongoing financial struggles that make them more vulnerable than larger facilities.67,68 When a hospital closes in a rural area, the impact is far more severe than in cities because residents lose one of their only nearby options for care.68 Working with local leaders has been shown to help prevent closures.69,70
Rural residents also face greater financial barriers. From 2010 to 2019, rural counties were older, less affluent, and had fewer health resources—and higher mortality rates—than urban counties.43 There is also a gap in insurance coverage. In 2023, 12.2% of people under age 65 in rural counties were uninsured, versus 10.8% in urban areas.71,72
Preventive care is harder to access in rural Tennessee. Residents are more likely to:
- Express vaccine hesitancy 60
- Have lower HPV vaccination rates 23
- Experience delayed HIV diagnosis 61
Limited access to specialists and mental health care also affects outcomes. Among people who died of drug overdoses with a mental health diagnosis, those in rural areas were more likely to live in mental health provider shortage areas.73 A lack of trust can further discourage care, even when facilities are available.20 During the COVID-19 pandemic, rural counties had higher mortality rates than urban ones, showing how access challenges can become life-threatening.74
-
Community-Driven Solutions
Community-driven solutions are practical steps that local partners can take together to improve access to high-quality health care. These actions are evidence-based, can be put in place quickly, and focus on the most important health care needs in each community.
- Promote services offered by local health departments. For example, the Community Health Access and Navigation in Tennessee (CHANT) program
helps families connect to needed services. CHANT staff help people find and set up
care, such as:
- Dental care
- Primary care (regular doctor visits)
- Vaccines
- Mental and behavioral health care
- Pregnancy and postpartum support
- Social services like housing or food help
- Visit the TDH CHANT page to learn more.
- Offer learning sessions about SNAP, WIC, TennCare (Medicaid), CoverKids(CHIP), and other benefit programs. Many people miss out on help simply because they don’t know what’s available. Community events that explain these programs in plain language can support family health and financial stability.
- Provide training on person-centered and culturally appropriate care. Health Councils or other groups can host training sessions to teach health workers
how to respect diverse backgrounds, languages, and needs. This builds trust between
providers and the community.
Talk with local health care providers about hiring interpreters. If community members speak different languages, having interpreters helps prevent misunderstandings and ensures everyone gets the care they need. - Encourage workplaces and health organizations to use trauma-informed policies. Trauma-informed workplaces treat people with care and understanding, recognizing that many have faced difficult life experiences. When organizations follow these policies, they provide safer and more supportive care.
- Join or support Patient and Family Advisory Councils. These councils provide opportunities for health care organizations to understand the perspectives of patients and families and build trust between patients, families, and providers. Because a patient’s health affects more than just the patient, successful family engagement can support the health and well-being of the entire family.
- Support free or sliding-scale clinics. Clinics that offer low or no-cost care help people without insurance or who can’t afford high medical bills. Sharing information about these clinics—or helping them grow—can make health care more accessible for everyone.
- Offer transportation support for medical appointments. Many people miss doctor visits because they don’t have a ride. Communities can partner with churches, nonprofits, or ride services to help people get to appointments.
- Host mobile health clinics or health fairs. Bringing health services directly to neighborhoods makes care more accessible. Mobile clinics can provide checkups, vaccines, and screenings in schools, churches, or community centers.
- Partner with schools to provide school-based health services. School nurses and school-based clinics help students get care without leaving campus. Communities can support these programs or help add services like mental health counseling or dental screenings.
- Start or support peer support groups. Groups for new parents, people managing diabetes, addiction recovery, or mental health can help people feel less alone and share resources.
- Promote mental health hotlines and crisis services. Posting support line numbers at community centers, libraries, and workplaces helps people know where to turn when they’re struggling.
- Create or share easy-to-read health guides. Plain-language flyers or videos about managing stress, knowing when to go to the ER vs. urgent care, or how to refill prescriptions can empower families to take charge of their health.
- Promote services offered by local health departments. For example, the Community Health Access and Navigation in Tennessee (CHANT) program
helps families connect to needed services. CHANT staff help people find and set up
care, such as:
-
Making Change Through Policies and Systems
Policy and system changes help improve access to high-quality health care over time. These evidence-informed actions strengthen health systems and make it easier for individuals and families to get the care they need.
- Support better screening in health care for common barriers. Many people struggle to get treatment because of things like cost, lack of transportation, or housing issues. Asking patients about these needs can lead to changes that will make health care access easier to obtain. Communities can also partner with schools and nonprofits to make attending these screenings easier.
- Encourage hospitals and clinics to ask patients for feedback. Simple exit surveys or follow-up emails can reveal problems and lead to solutions. Health Councils can promote continuous evaluation so that agencies know how to improve the experience.
- Work with local nonprofit hospitals to align community goals. Nonprofit hospitals are required by law to complete a Community Health Needs Assessment (CHNA) every three years. Communities often create their own Community Health Assessment (CHA). Bringing these two efforts together helps hospitals and residents focus on the same goals instead of working separately.
- Find funding to improve telehealth and internet access. Telehealth lets people meet with doctors by phone or video. This is especially important in rural areas where clinics are far away. Helping families get devices and internet access makes virtual care easier to use.
- Encourage health care groups to get involved in community advocacy. Health clinics and hospitals can push for safer roads, sidewalks, and bike lanes so people have better ways to travel to appointments and stay active. When health organizations speak up, local leaders are more likely to listen.
- Support policies that focus on the root causes of health problems. Instead of only treating health issues after they happen, communities can study why these problems start. Conduct a root cause analysis to explore the factors contributing to a particular health challenge for communities. Analyzing root causes can help communities identify and tackle the underlying causes of health issues.
- Encourage clinics and hospitals to share data and work together. When health care providers, schools, and social service agencies share information (while protecting privacy), they can better coordinate support for families. This reduces gaps in care and prevents people from falling through the cracks.
-
Community Spotlight
The Health Council Community of Practice (CoP) connects Tennessee Health Councils through shared learning and discussion around health priorities. The links below provide access to recent CoP conversations related to this topic. To learn more about the Community of Practice, click here.
Trousdale County (January 2024)
Grundy County (September 2025)
Submit your own Community Spotlight! Please email Health.Councils@tn.gov with any relevant stories, resources, or presentations related to this topic. -
Partners and Resources
Tennessee Department of Health
- Local Health Departments
All 95 counties in Tennessee have a local health department, and some larger counties have multiple health department facilities. These offices are ideal partners for health councils to collaborate with to improve health in local communities. - Women, Infants, and Children Program (WIC)
WIC helps pregnant women, new mothers, and young children get healthy food, nutrition education, breastfeeding support, and referrals to doctors. It makes sure families have what they need during early childhood. - Community Health Access and Navigation in Tennessee (CHANT)
CHANT connects eligible families and individuals to medical care and support services through local health departments. They can help with things like finding doctors, coordinating care, and even helping with costs like co-pays. - Tennessee Healthy Smiles Initiative
- Smile on 65+ provides dental care and case management for older adults through a partnership with Interfaith Dental Clinic.
- Tennessee Dental Safety Net Denture Program provides state funds to help with the cost of dentures for working-age adults (18-64) seen in charitable care clinics.
Tennessee Division of TennCare
- TennCare
The state’s Medicaid program provides health insurance to Medicaid-eligible individuals and families. - Presumptive Eligibility (PE)
This program provides immediate temporary TennCare coverage for eligible pregnant women and individuals diagnosed with Breast and/or Cervical Cancer. - CoverKids
Tennessee’s CHIP program provides health insurance for children aged 18 and younger and pregnant women who meet eligibility requirements. - Health Starts Provider Partnerships
TennCare works with health care providers to screen patients for non-medical needs like food, housing, or transportation. When a need is found, providers connect patients to local community organizations and follow up to make sure they received help. These partnerships also collect data to learn what works best so that support can be expanded across the state.
Tennessee Department of Disability and Aging
- Tennessee State Health Insurance Assistance Program (TN SHIP)
This federal funding program provides free, unbiased counseling and assistance to Medicare-eligible adults, their families, and caregivers. Trained counselors can assist with all Medicare-related questions at 1-877-801-0044 or by email at mailto:dda.ship@tn.gov
Tennessee Department of Mental Health and Substance Abuse Services
- Project Rural Recovery
The program uses four mobile clinics to deliver free behavioral and physical health services in rural, underserved, or distressed areas. Currently, the program operates in 20 counties thanks to partnerships with the McNabb Center in Middle Tennessee, Buffalo Valley Inc. and Ridgeview Behavioral Health Services in East Tennessee, and Ridgeview Behavioral Health in West Tennessee. - Behavioral Health Safety Net (BHSN)
The BHSN program provides mental health care for Tennesseans age 3 and older who have no behavioral health insurance and meet program criteria. Services include therapy, psychiatric medication management, case management, and help with labs, pharmacy, transportation, and peer support. BHSN providers serve all 95 counties, either in person, in nearby counties, or through telehealth.
Other Tennessee Resources
- Tennessee Charitable Care Network (TCCN)
This network of nonprofit charitable clinics and programs provides free or reduced-cost medical, dental, and mental health services for Tennesseans in need. - Tennessee Alliance of Oral Health Advocates (TNAOHA)
TNAOHA’s Safety Net Dental Clinic Directory provides a list of dental clinics based on varying levels of patient insurance acceptance. - Insure All Tennessee
This non-profit offers free help for all Tennesseans looking to enroll in TennCare, CoverKids, Federal HealthCare Marketplace Insurance Plans, CoverRx, and other health benefits.
- Local Health Departments
-
To Learn More
Center for Health Care Strategies
- Trauma-Informed Care Implementation Resource Center
This website includes resources on multiple topics under the umbrella of TIC, including how to invest in a trauma-informed workforce.
Department of Health and Human Services
- Healthy People 2030
This national initiative uses data-driven goals to improve health and well-being by focusing on the Social Determinants of Health. The website provides evidence-based objectives and resources to guide efforts in improving health care access and quality. - Think Cultural Health
This HHS website provides tools and training on culturally and linguistically appropriate services, health equity communications, and policies regarding cultural competency.
National Institute for Health care Management
- Rural Health: Addressing Barriers to Care
This webpage provides insightful infographics on the state of health care access in rural America.
The Picker Institute
- The Picker Principles of Person-Centered Care
This resource describes the eight elements of PCC in depth, with additional resources and research.
SAMSHA
- Key Ingredients for Successful Trauma-Informed Care Implementation
This issue brief outlines important elements of implementing TIC approaches in organizations and clinical practices.
- Trauma-Informed Care Implementation Resource Center
 Stout Drive Road Closure
Stout Drive Road Closure