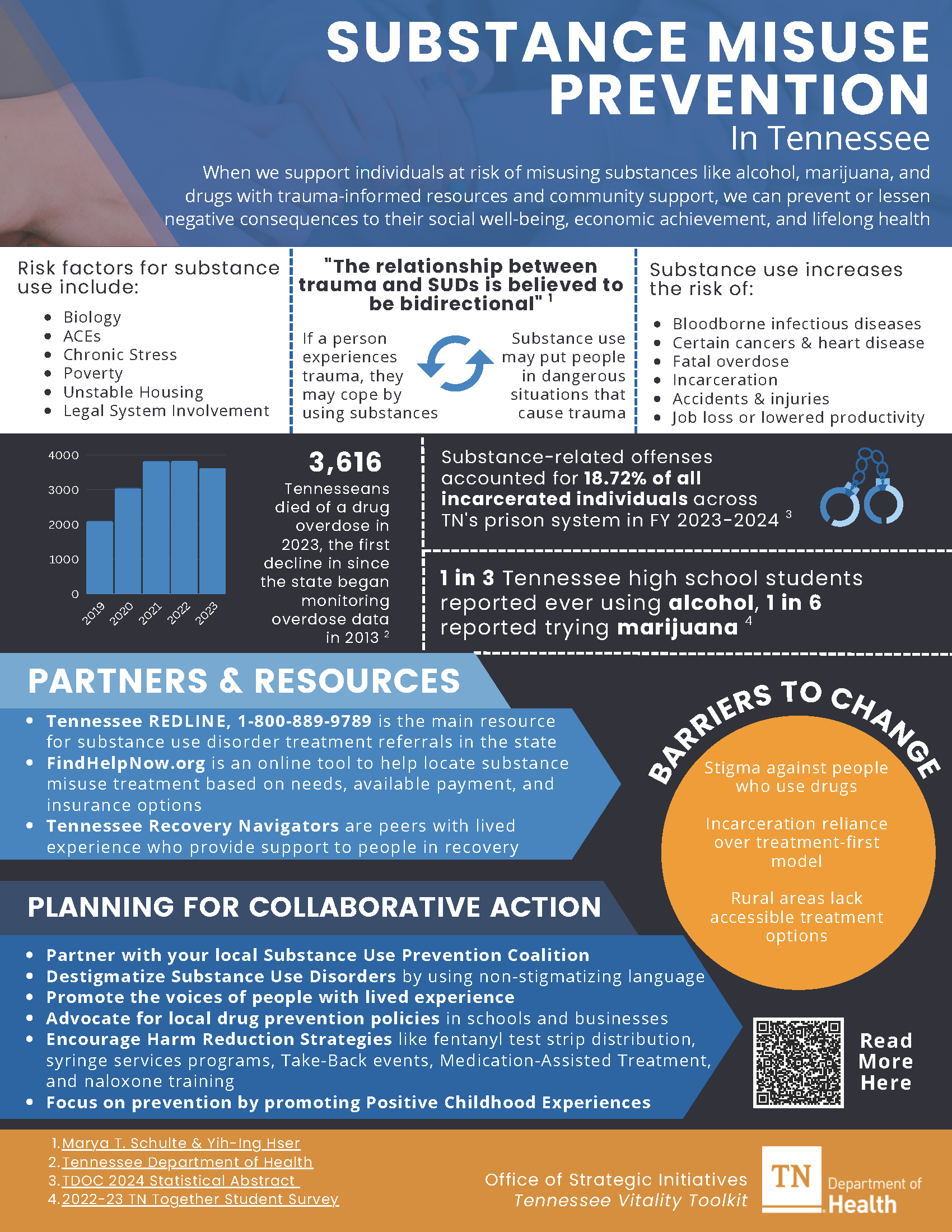
Substance Misuse Prevention
Every year, thousands of people in Tennessee are affected by substance use. Factors like job loss, stress, and lack of access to mental health care have made the problem worse. Using substances such as opioids, alcohol, and stimulants can cause serious harm to a person’s body, mind, and relationships.
Substance use continues to have a significant impact on communities across Tennessee. While some recent trends show minor progress, the overall impact remains serious. For example:
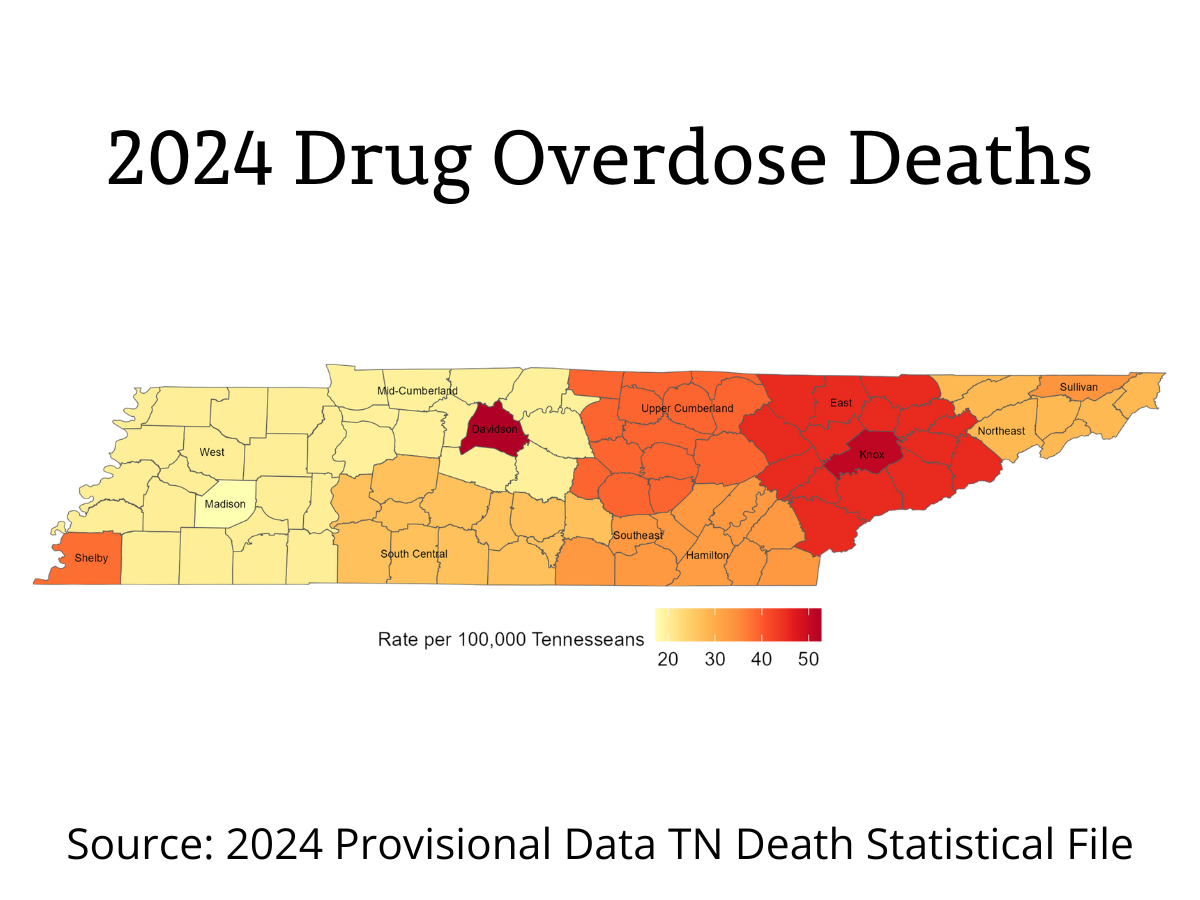
- In 2024, 2,473 Tennesseans lost their lives to drug overdoses, based on early state data. This marks a major improvement from recent years, showing progress in the fight against substance-related deaths across the state.1
- Most overdose deaths in 2024 involved opioids, especially illicit fentanyl, which continues to drive many fatal overdoses. Deaths linked to stimulants like meth and cocaine went down overall, but xylazine, a strong sedative sometimes mixed with opioids, showed up in more deaths than before.1
- All parts of the state saw fewer overdose deaths in 2024, though the Nashville-Davidson and Knox Metro regions continued to have the highest rates. 1
Having fair, judgment-free access to treatment and coordinated care is essential for helping people recover and reducing the harm caused by substance use. Many Tennessee communities already have strong partnerships, such as Substance Use Prevention Coalitions (SUPCs), that dedicate their time and resources to building healthier, safer communities.
County Health Councils (CHCs) can strengthen this work by promoting prevention programs, connecting people to local resources, and fostering a culture that supports treatment rather than punishment. To make sure everyone has the chance to be healthy and thrive, communities must work to reduce stigma and treat people who use substances with compassion and respect.
-
Why is Prevention and Treatment of Substance Use/Misuse Important for Community Well-Being?
Substance use and misuse can have a profound impact on individuals' health and well-being. Substance use is linked to mental health problems, poor nutrition, and social and legal challenges, as well as an increased risk of early death.2,3
People experience challenges with substance abuse for many reasons, making it a complex issue that affects individuals, families, and communities.4 These challenges are often shaped by the conditions in which people live, work, and learn. Social determinants of health, including income, housing, education, and access to care, are among the most significant risk factors.5
When communities address these underlying social conditions, they can better target the root causes of substance use.5
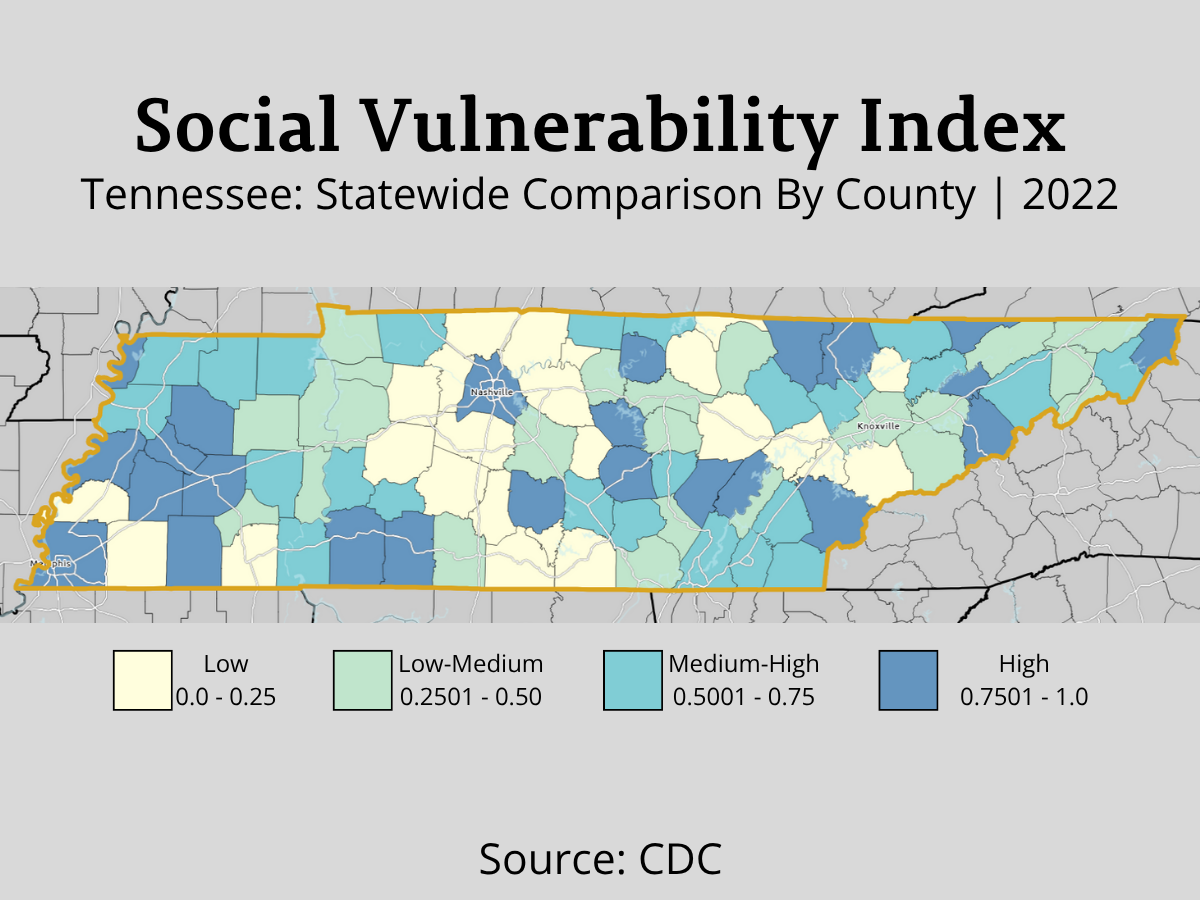
The Role of Social Vulnerability
The Social Vulnerability Index (SVI) measures the impact of social and economic factors on a community’s ability to respond to challenges.6 Research shows that counties with higher SVI scores—meaning they face more economic and social hardships—tend to have higher rates of drug overdose deaths.7 Most Tennessee counties have medium-high or high SVI scores, putting them at greater risk for substance use and misuse.8
How Substance Use Affects the Body and Mind
Substances can have powerful effects on the brain and body. They can alter brain function, resulting in changes in mood, behavior, and thought patterns.3 Substance use is closely connected to mental health. Many people turn to substances to cope with long-term stress, violence, unemployment, unstable housing, or Adverse Childhood Experiences (ACEs). Over time, this can make their mental health worse and lead to substance use disorder.
Sadly, stigma—from individuals, families, healthcare providers, or the community—often prevents people from seeking help.9 Long-term substance use can also make it harder for a person to enjoy daily life without substances. As tolerance builds, more of the substance is needed to feel the same effects, raising the risk of health problems and overdose.
The Economic and Community Costs
Substance use also carries a heavy financial burden. Substance misuse costs Tennessee around $2 billion annually, including $1 billion in lost workforce productivity.10 Incarceration adds to these costs. Alcohol and drugs are implicated in an estimated 80% of offenses leading to incarceration in the United States.11 According to the Tennessee Bureau of Investigation (TBI), the state recorded 46,742 drug/narcotic violations and 20,941 DUI arrests in 2024.12
Building Healthier, Stronger Communities
To make real progress, communities must provide trauma-informed, non-stigmatizing treatment options so people can get help without fear or shame. When local partners work together to address the social conditions that lead to substance misuse—such as poverty, lack of opportunity, and limited access to care—everyone benefits.
-
What are the Disparities?
Any person can develop a substance use disorder (SUD), but certain groups may be more likely to develop SUDs and can face barriers when it comes to finding treatment.
Adolescent Teens
Alcohol and drug use often begin during the teen years, with some children starting as young as 12.13 According to the Centers for Disease Control and Prevention (CDC), most adults with substance use disorders first started using when they were teens or young adults.14 Teens who misuse alcohol or drugs are also more likely to experience physical and mental health problems.14
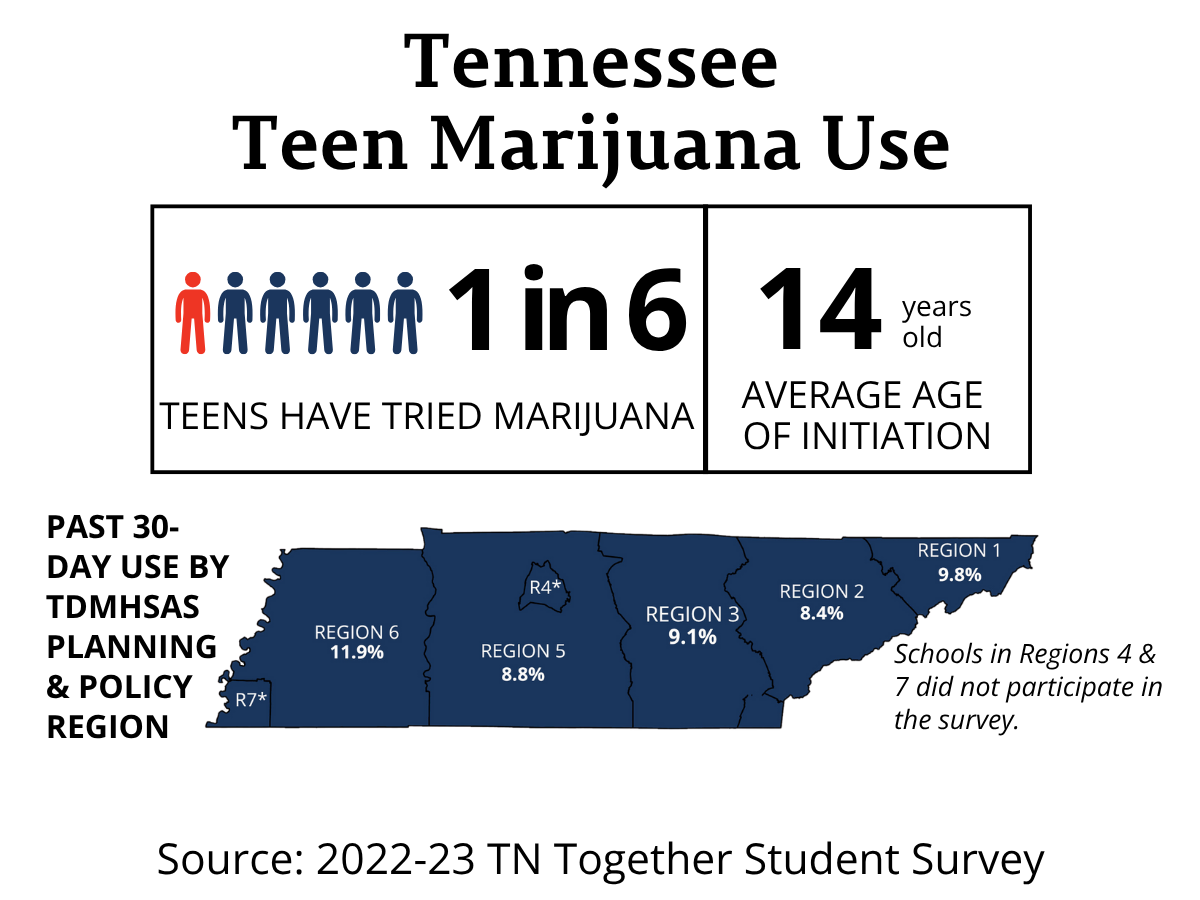
The 2022–23 TN Together Student Survey revealed public school students’ behaviors, attitudes, and social norms related to alcohol and drug use. The survey conducted by the Tennessee Department of Mental Health & Social Services (TDMHSAS) included more than 23,000 public school students in eighth, tenth, and twelfth grades across 35 counties. 15
Alcohol is the most commonly used substance among Tennessee teens. About one in three students (30.6%) said they have tried alcohol, with the average first use at age 13.4.16 Nearly one in four students (24.2%) reported drinking alcohol in the past 30 days, and 11.1% said they drank on six or more days during that time. Most students recognize that drinking regularly is not acceptable.16 Most students, 88.4%, said it would be wrong for someone their age to drink every day, and 95.2% believe their parents would strongly disapprove.16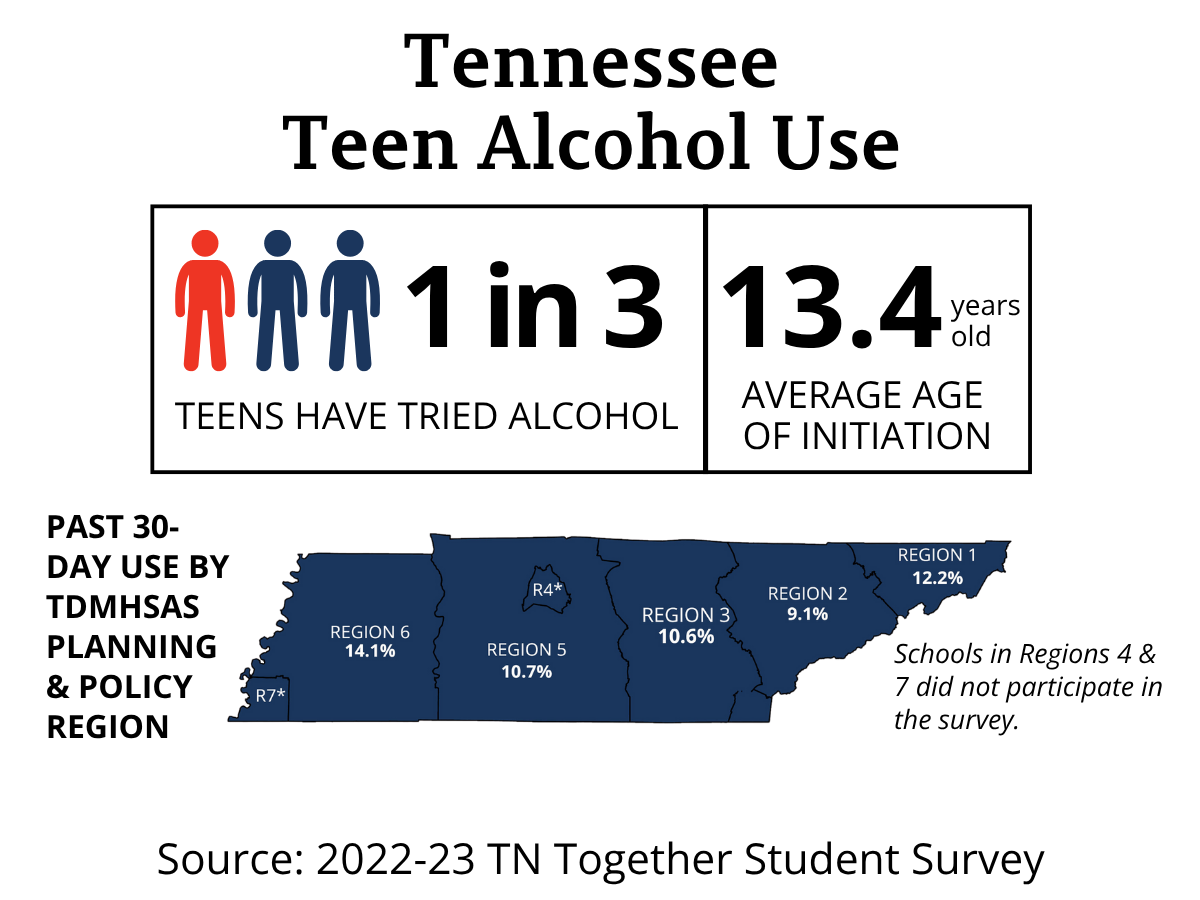
About one in six students (16.8%) in Tennessee have tried marijuana, with the average first use at age 14.17 Among those who used marijuana in the past 30 days, one in two students (53.4%) said they used it on six or more days.17 Most Tennessee teens, 79.9%, believe using marijuana is wrong; 90.9% said their parents would strongly disapprove.17
These findings show the importance of early prevention, parent–teen communication, and community support in reducing youth substance use. When teens understand the risks and feel supported by their families, schools, and peers, they are more likely to make healthy choices.
Young Adults (ages 18 to 25)
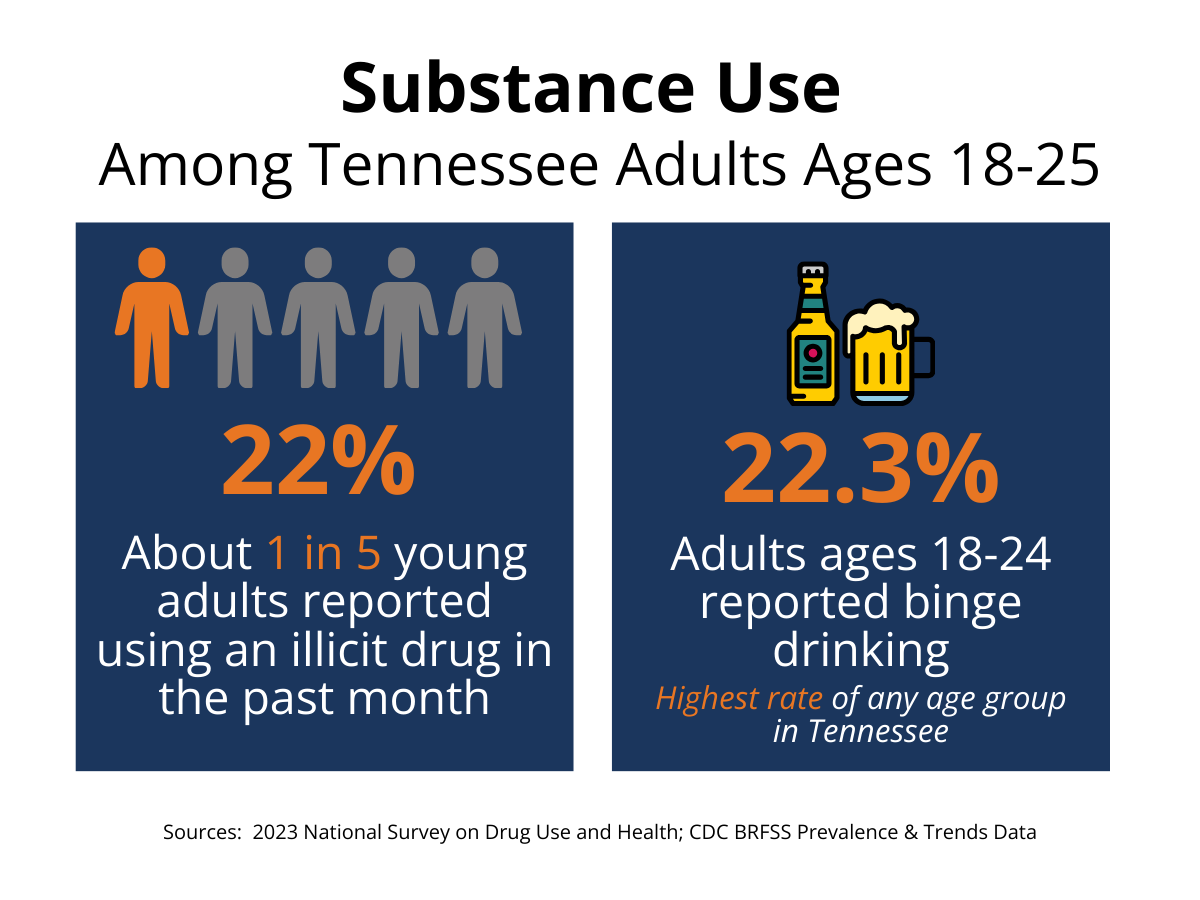
Many young adults in Tennessee are struggling with the effects of substance misuse. According to 2022–2023 estimates, about one in five Tennesseans aged 18–25 (22%) reported using an illicit drug in the past month.18 Binge drinking is also common in this age group. In 2023, 22.3% of adults aged 18–24 reported binge drinking, the highest rate of any age group in the state.19
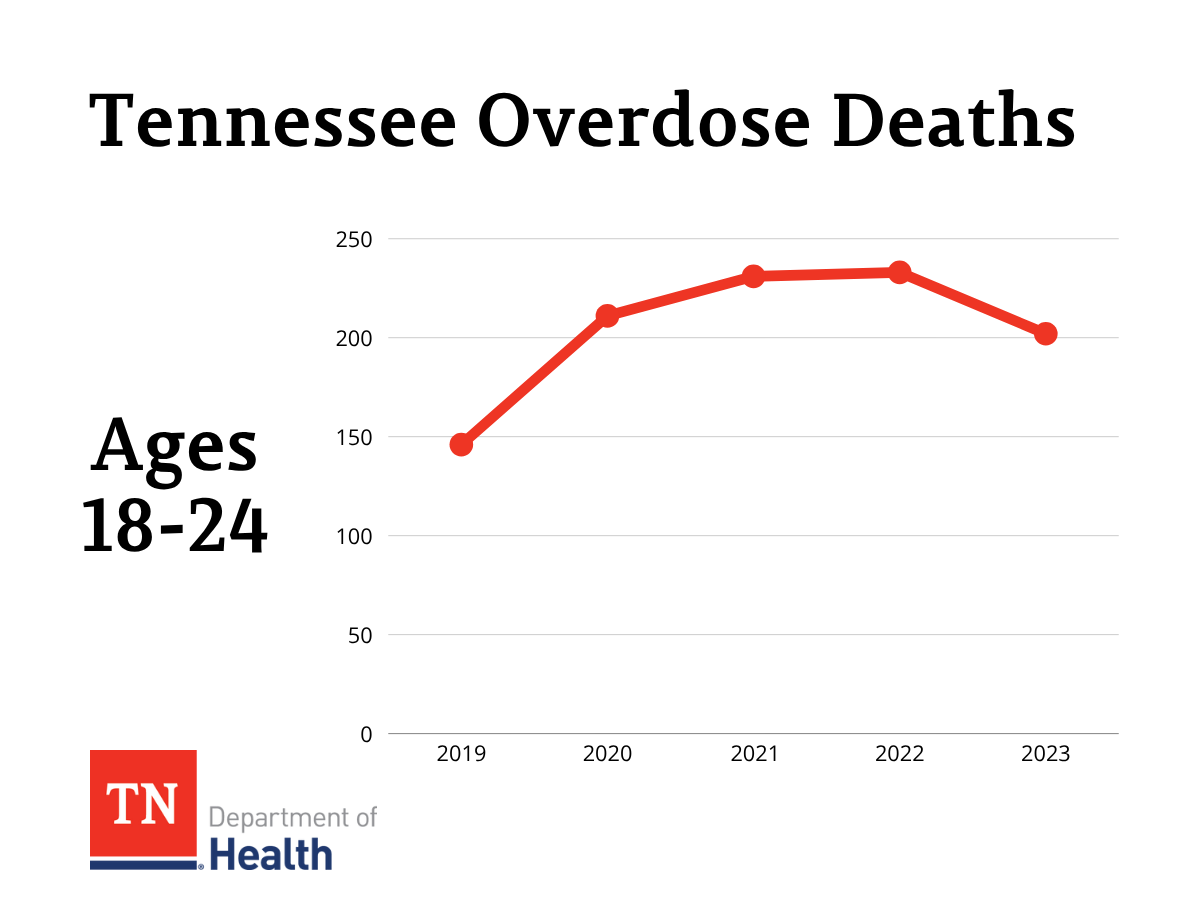
While many young adults experiment with drugs or alcohol, the impact can be serious. After several years of increases, overdose deaths among people ages 18 to 24 leveled off between 2021 and 2022 and then declined in 2023.20 This is a hopeful sign, but it is also a reminder that prevention and early intervention remain important for this age group.
Substance misuse is closely tied to mental health. Research suggests that cannabis use in young adults is linked to anxiety and depression. Over time, substance misuse and mental health concerns can interact in ways that make both more severe. 21 Supporting young adults with both mental health care and substance misuse prevention can help build healthier futures.
Older Adults
Substance misuse can be a serious concern for older adults. As people age, they are more likely to live with chronic health conditions and take multiple prescription medications. This can increase the risk of SUD or accidental misuse of medications.22 Because health problems and medication side effects can mimic symptoms of substance use, SUD can be harder to recognize in older adults.
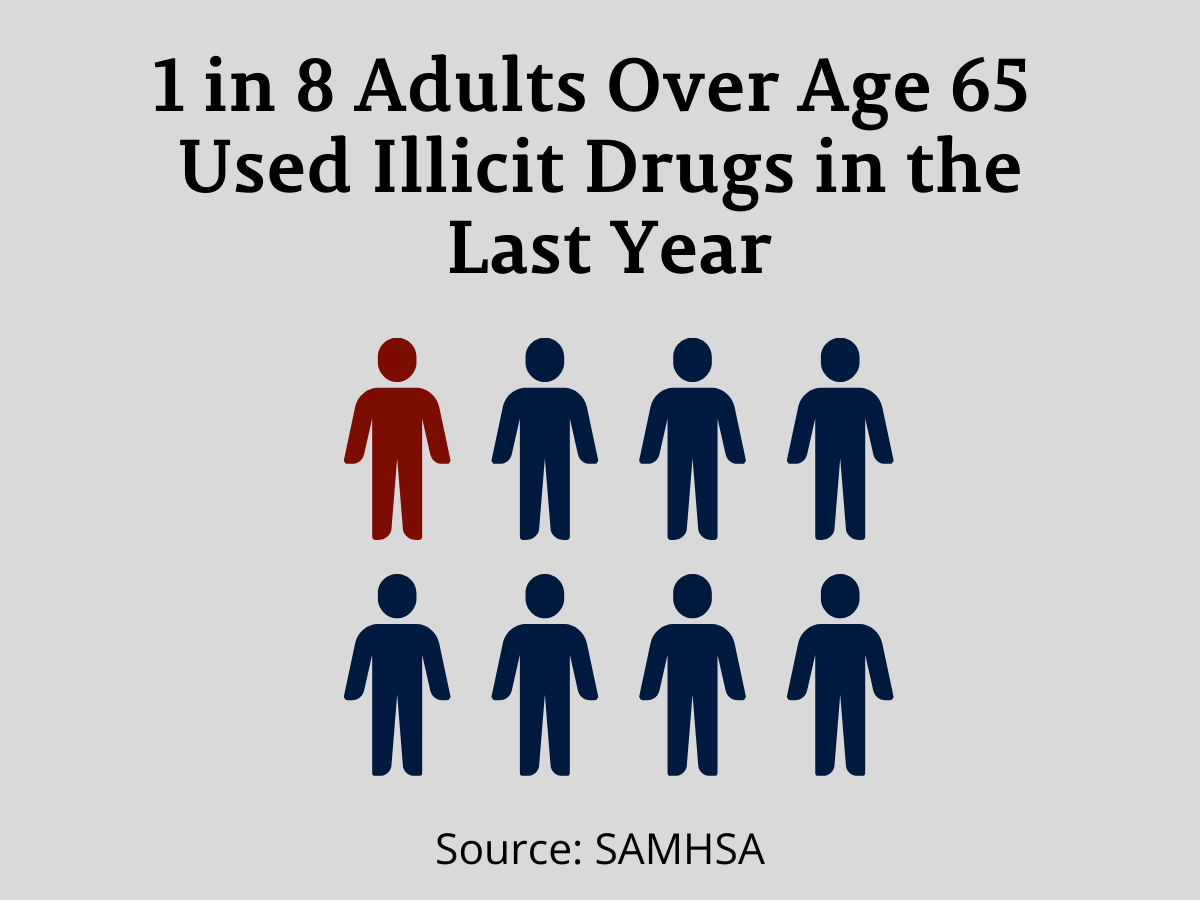
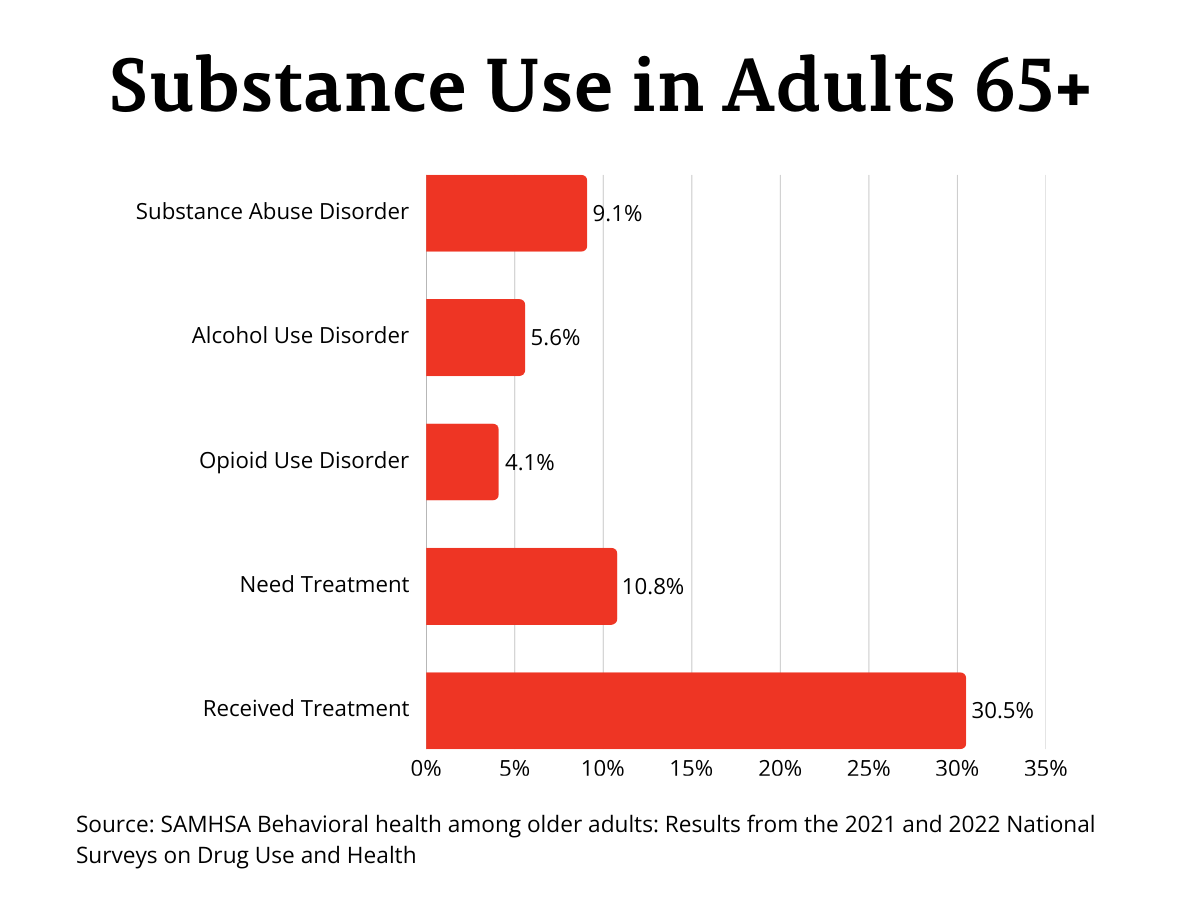
National estimates show that one in eight (12.1%) used illicit drugs in the last year, and one in 11 (9.1%) had a substance use disorder.23 Alcohol use disorder affected about one in 25 older adults (5.6%), while opioid use disorder affected one in 50 (4.1%).23 About one in nine (10.8%) older adults reported needing substance use treatment, but only one in three (30.5%) of those who needed treatment received it.23
Incarcerated Individuals
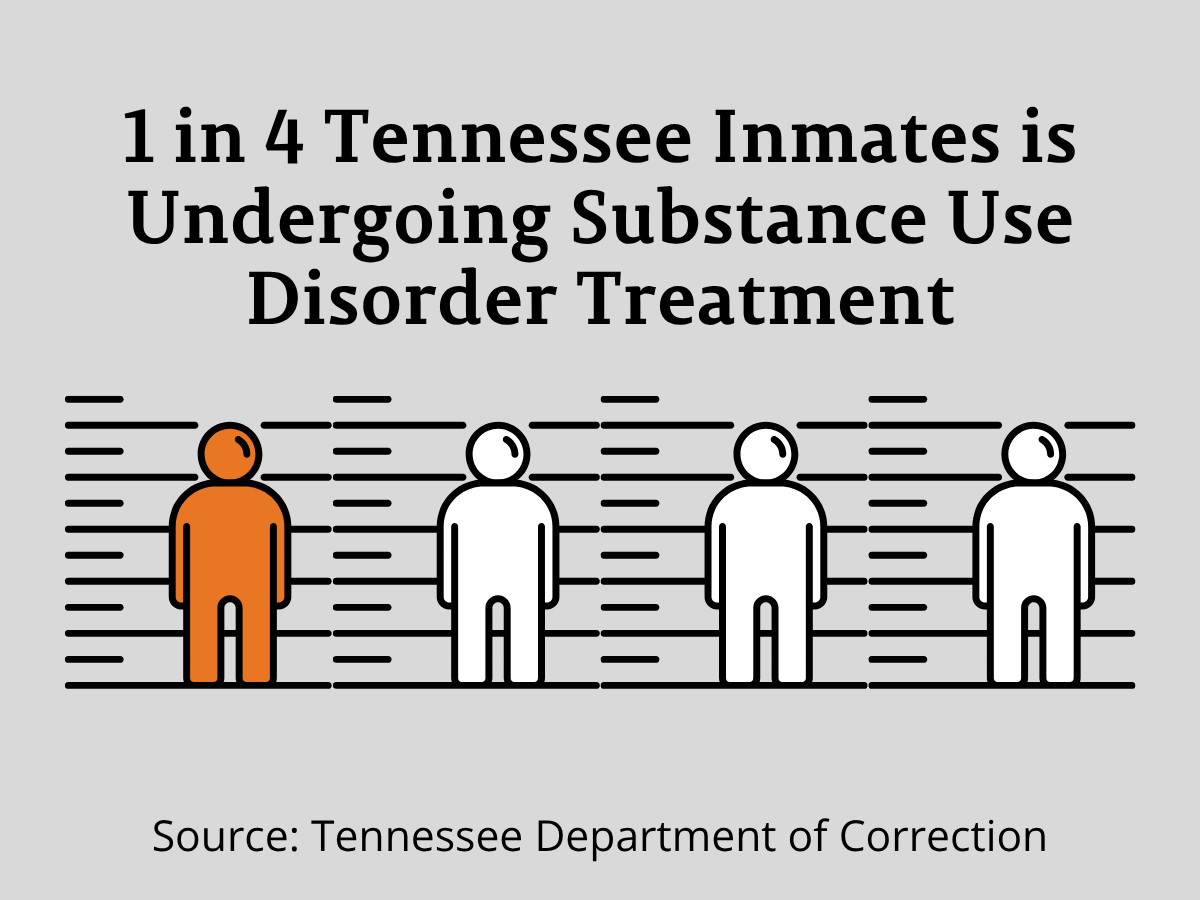
Substance misuse and incarceration are closely connected. In the United States, one in five people in jail is there due to drug offenses.24 According to the Tennessee Department of Correction (TDOC), the most common mental health diagnosis they encounter is alcohol and substance use disorder. TDOC officials report that nearly one in four Tennessee inmates is undergoing treatment for substance use disorder.25
Programs that help people rebuild their lives after incarceration, known as re-adaptation interventions, can make a significant difference. These programs lower the risk of opioid overdose after release and increase the chances of a successful re-entry into society.26
However, people who have been incarcerated often face stigma, both from within themselves and from their communities. This stigma can make it harder to seek help, showing the need for tailored treatment and support programs that focus on compassion and recovery.27 People with both a SUD and mental health conditions face even greater challenges. These individuals are at a higher risk of returning to prison, which highlights how important it is to provide access to mental health care, SUD treatment, and strong family and community support.28
Individuals with Disabilities
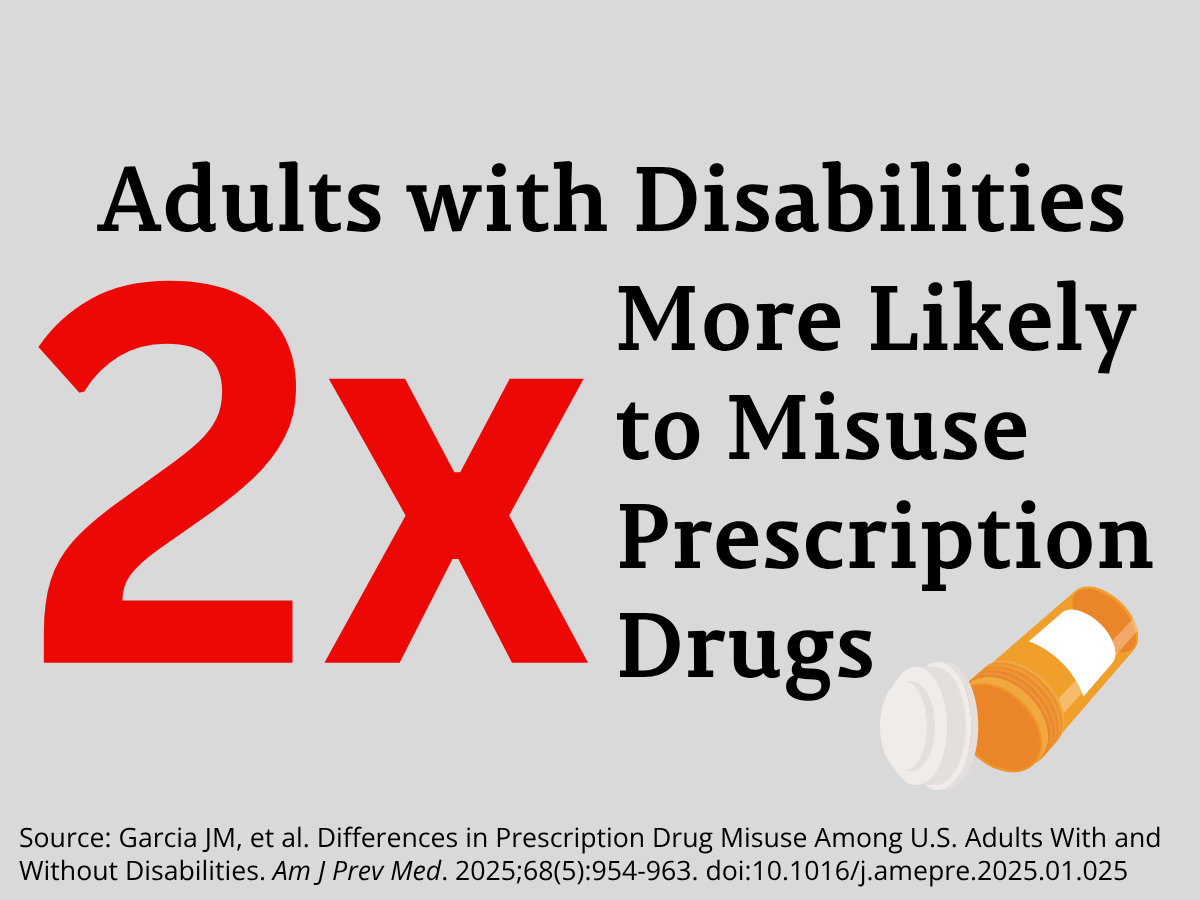
People with disabilities have a nearly 50% greater chance of having a substance use disorder than those without disabilities.29 People with disabilities are also twice as likely to misuse prescription drugs when compared to adults without disabilities.30 As many as 70% of people with disabilities with substance use disorder say they are not getting the treatment they need.31
The most significant barriers to treatment for individuals with disabilities are cost and stigma.31 These challenges can worsen during public health emergencies, such as the COVID-19 pandemic, when access to care is more limited.32
LGBTQ+ Individuals
National data shows that substance misuse is high among sexual minorities, people who identify as lesbian, gay, bisexual, or another non-heterosexual identity. According to the 2023 National Survey on Drug Use and Health, sexual minorities are more likely to use illicit drugs and marijuana than straight people.33 LGBTQ+ individuals are also likely to use multiple substances compared to people who identify as heterosexual.34
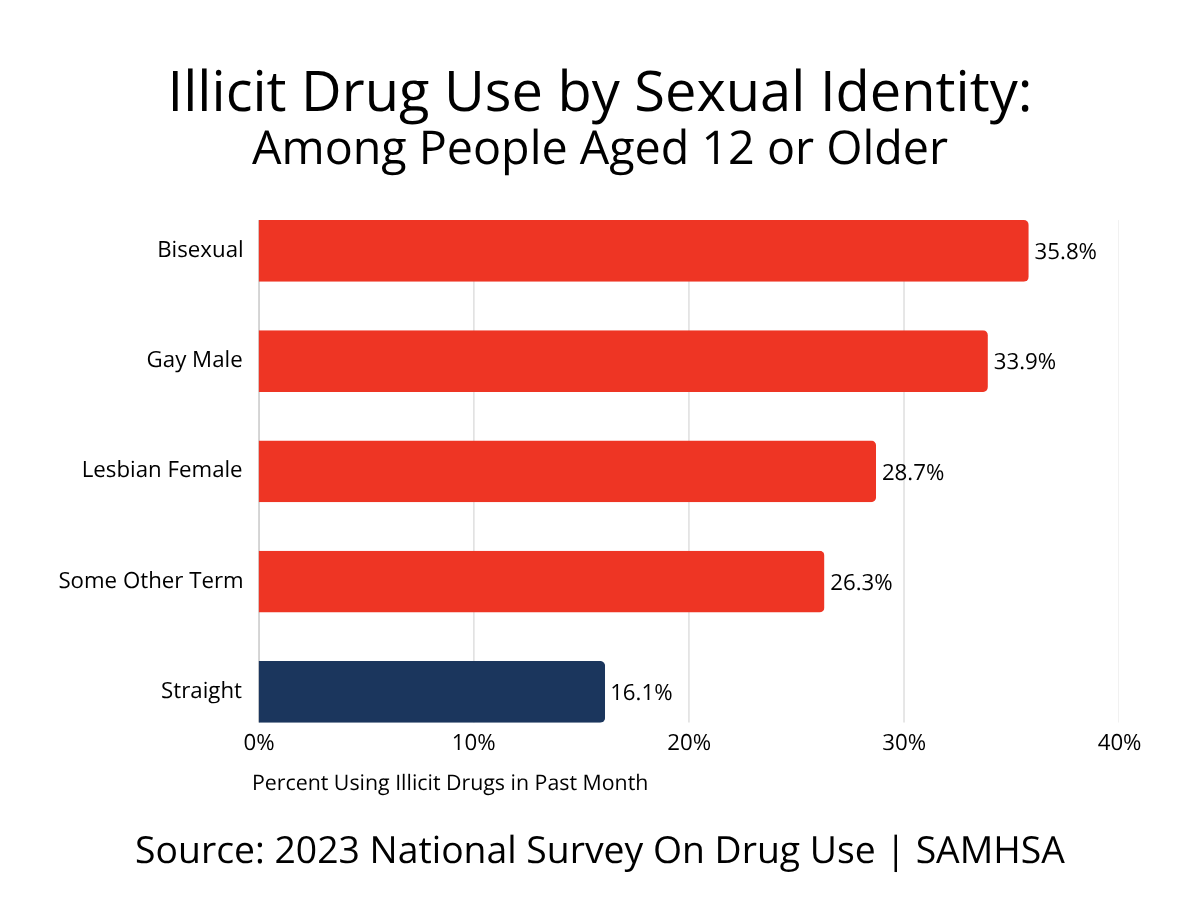
LGBTQ+ individuals are more likely to seek treatment for SUD; however, they also face more barriers to care.35–37 Sexual minorities, especially young adults, are at a higher risk of co-occurring mental health conditions due to factors like stigma, discrimination, and social stress.38 However, few programs are designed to meet their unique needs. One national study found that less than one-third of medication for opioid use disorder (MOUD) facilities offer LGBTQ-specific services.39
LGBTQ+ individuals also tend to experience greater social and economic challenges, which can increase their risk for substance misuse or make it harder to access treatment.40
Pregnant Women
Substance use during pregnancy can cause serious health problems for both the mother and baby. Care for pregnant women with substance use disorder requires special attention. Opioid exposure during pregnancy has been linked to preterm labor.41,42
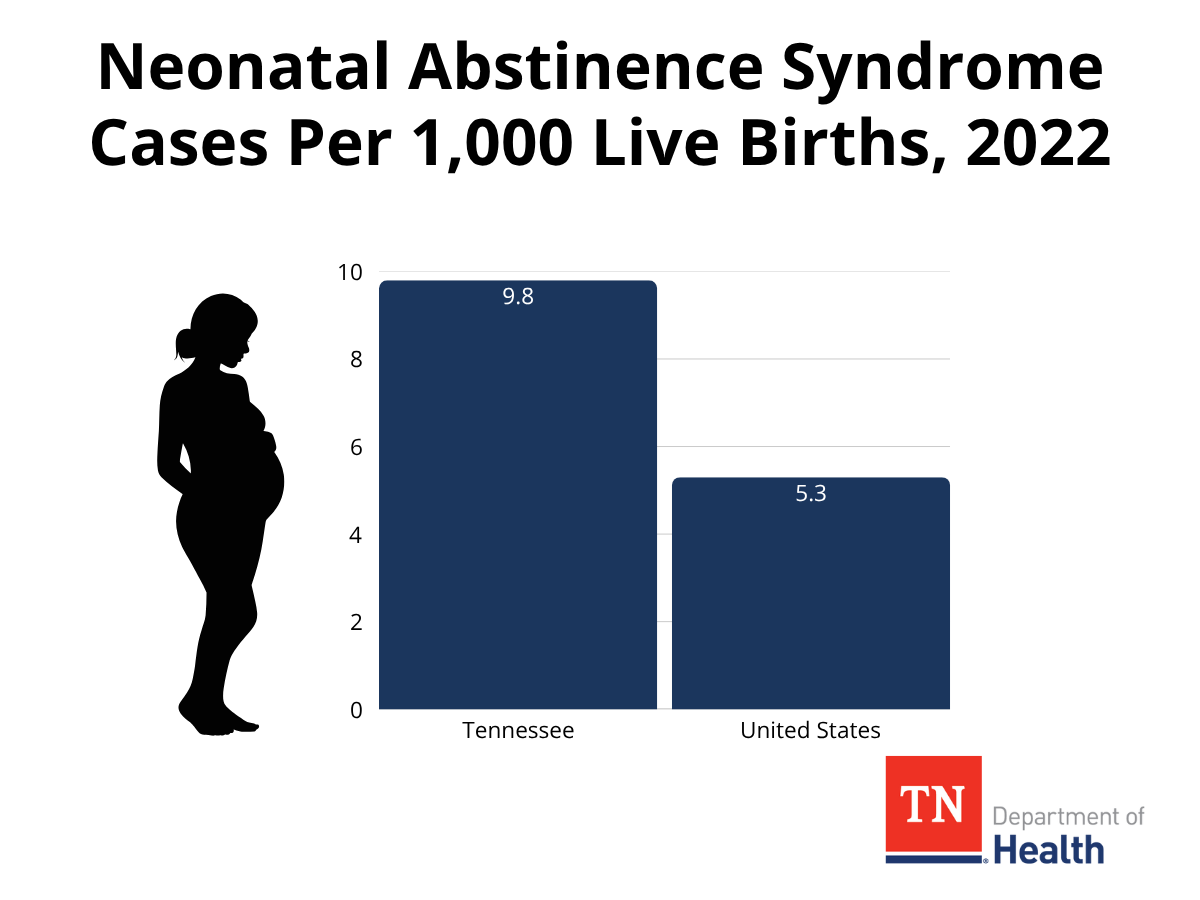
Opioid Use Disorder (OUD) has been linked to higher rates of infant death.43 Babies exposed to opioids before birth may develop Neonatal Opioid Withdrawal Syndrome (NOWS), which causes withdrawal symptoms shortly after delivery.44 NOWS is a specific type of Neonatal Abstinence Syndrome (NAS), which refers more broadly to withdrawal from any substance, not just opioids. 45 In 2022, Tennessee had a higher rate of NAS—9.8 cases per 1,000 live births—compared to the national average of 5.3.46 Nearly half (46.4%) of NAS cases from that year included the use of illicit drugs.46 More than half of the women (53%) whose infants were diagnosed with NAS had not received enough prenatal care.46
Treatment for opioid use disorder during pregnancy, such as buprenorphine therapy, can significantly improve health outcomes for both mothers and babies.47 It also lowers the risk of preterm birth.48 However, many pregnant women still face barriers to care, including stigma and lack of access to treatment.49,50 From 2009 to 2016, 72% of pregnant women in Tennessee with a likely OUD diagnosis did not receive needed treatment.48
Racial and Ethnic Minorities
Across Tennessee, many minority communities are feeling the heavy impact of substance use and overdose, especially among Black and Hispanic residents. State data shows differences in both drug use and access to treatment across racial and ethnic groups.
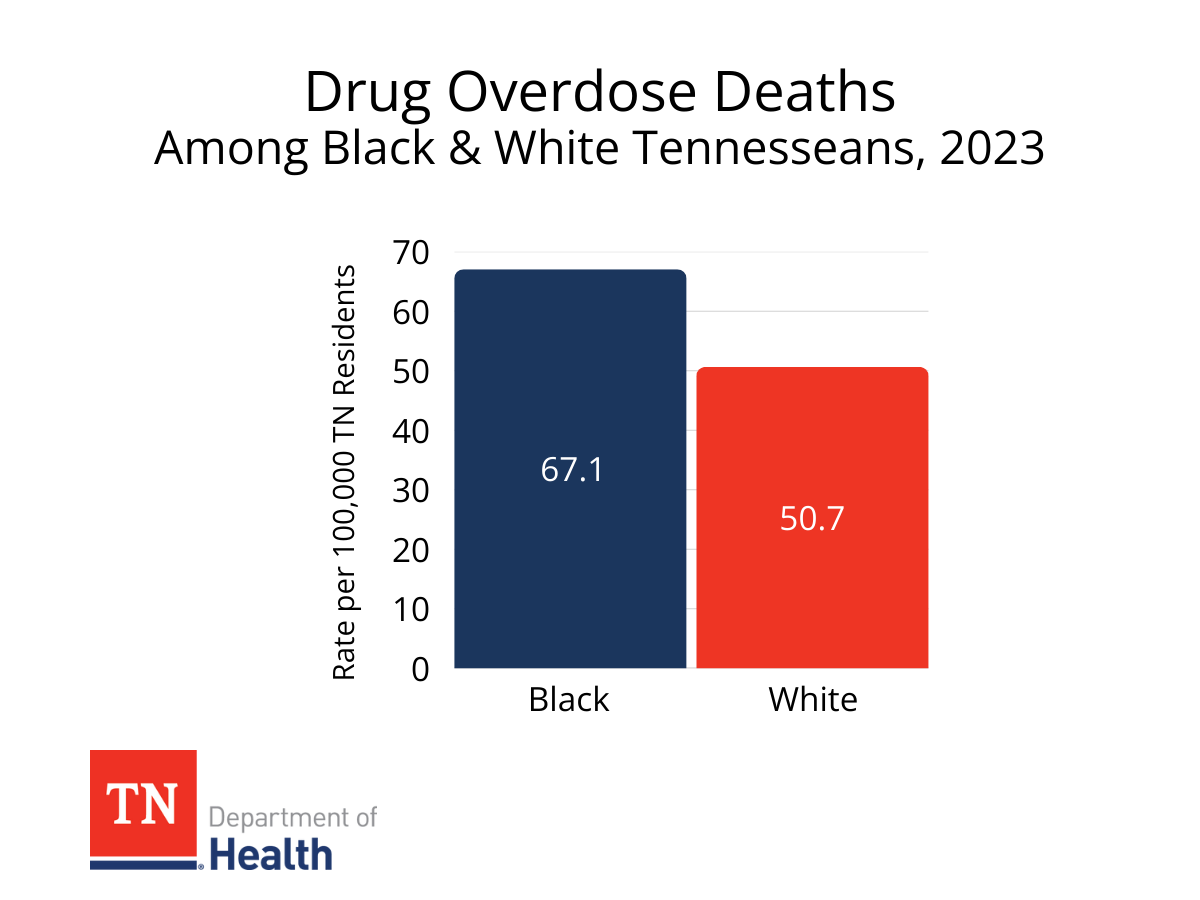
State data from 2023 shows that Black Tennesseans are dying from overdoses at higher rates than White Tennesseans, about 67 deaths for every 100,000 people compared to 51 for White residents.20 Most of these deaths involved fentanyl or stimulants like cocaine and methamphetamine. 20 In 2023, hospital data showed that Black Tennesseans had the highest rates of both outpatient visits and hospital stays related to drug overdoses.51 Hispanic Tennesseans have also seen a sharp rise in overdose deaths, climbing from 49 in 2019 to 120 in 2023.20
These numbers show that substance use and overdose do not affect everyone the same way. Many minority communities face greater barriers to treatment, fewer resources, and higher risks, making it especially important to continue culturally relevant prevention, education, and recovery efforts across the state.
Rural Communities
People living in rural communities often face additional challenges when it comes to getting help for substance use and mental health needs. Behavioral health services are not as widely available in rural areas as they are in cities, making it harder for someone with a substance use disorder to find treatment they can afford quickly.52 Without reliable transportation, it can be difficult—or even impossible—to attend healthcare appointments or return home safely. In smaller, close-knit communities, people may also hesitate to seek help because of stigma or fear of how others might respond.52
Studies show that these barriers have real effects. A national study from 2016–2018 found that patients in rural areas were less likely to begin or stay engaged in treatment for alcohol, opioid, or other drug use disorders.53 Rural Americans are also more likely to die from drug overdoses than people living in urban areas.54
Mental health concerns and substance use disorders often occur together.55 However, rural communities are less likely to have access to mental health services, which increases the adverse effects of substance use on individuals and families.56 Most rural hospitals also lack adequate behavioral health and substance misuse treatment options.57,58
Veterans
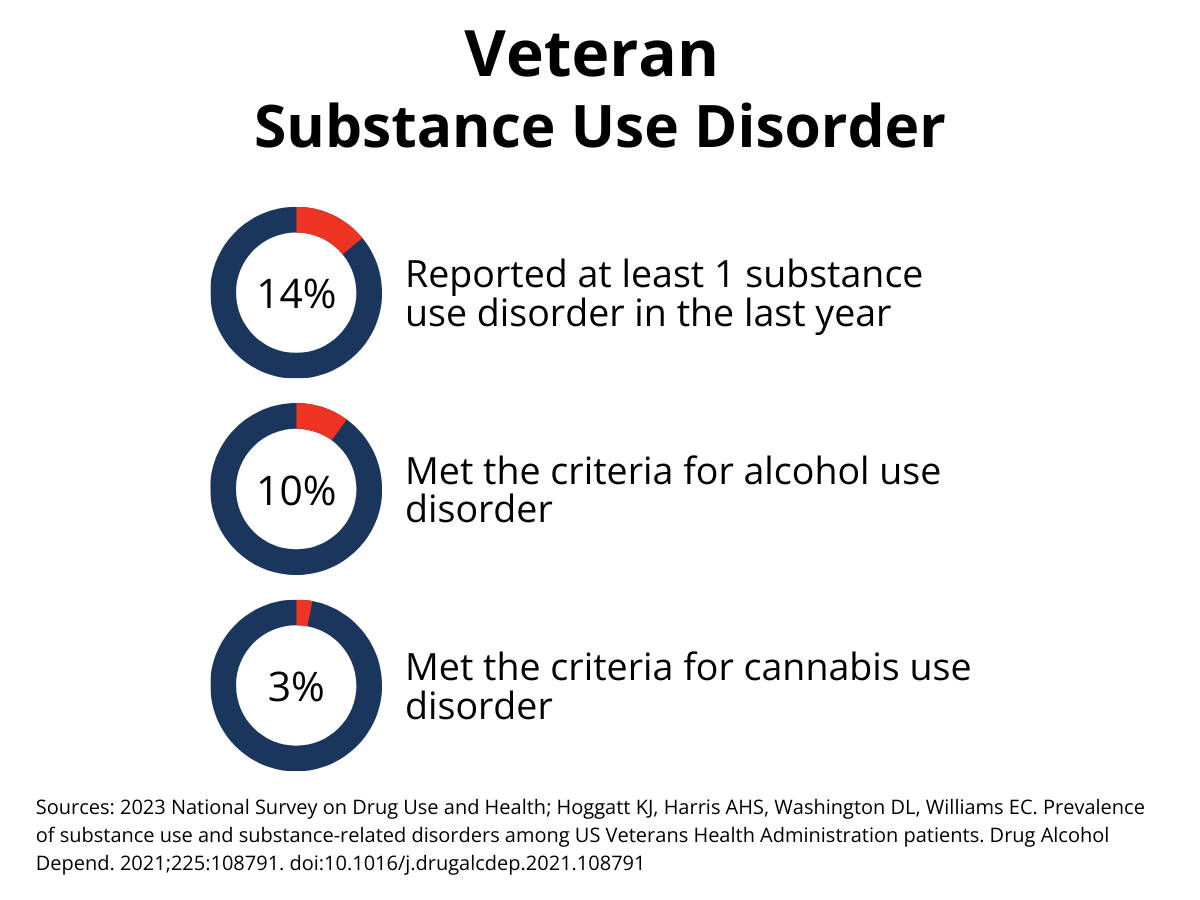
Veterans also experience distinct challenges related to substance use and mental health. The most common substances used by veterans are alcohol and marijuana. Some veterans may turn to these substances to cope with the mental health challenges that can come with military service.63,64
Overall, veterans have slightly higher rates of substance use disorder than the general population.63 In 2023, about 14% of U.S. veterans reported having at least one substance use disorder in the past year.65 Among Veterans Affairs (VA) patients, 10% met the criteria for alcohol use disorder, and 3% met the criteria for cannabis use disorder.66
Substance use among veterans taking prescription opioids is also a concern. One in four veterans on long-term opioid therapy has a diagnosed substance use disorder, showing the importance of regular screening and targeted interventions.67
Data from the U.S. Veterans Health Administration show that between 2005 and 2019, diagnoses of cannabis use disorder increased, especially among veterans living with chronic pain.68,69
Unhoused Individuals
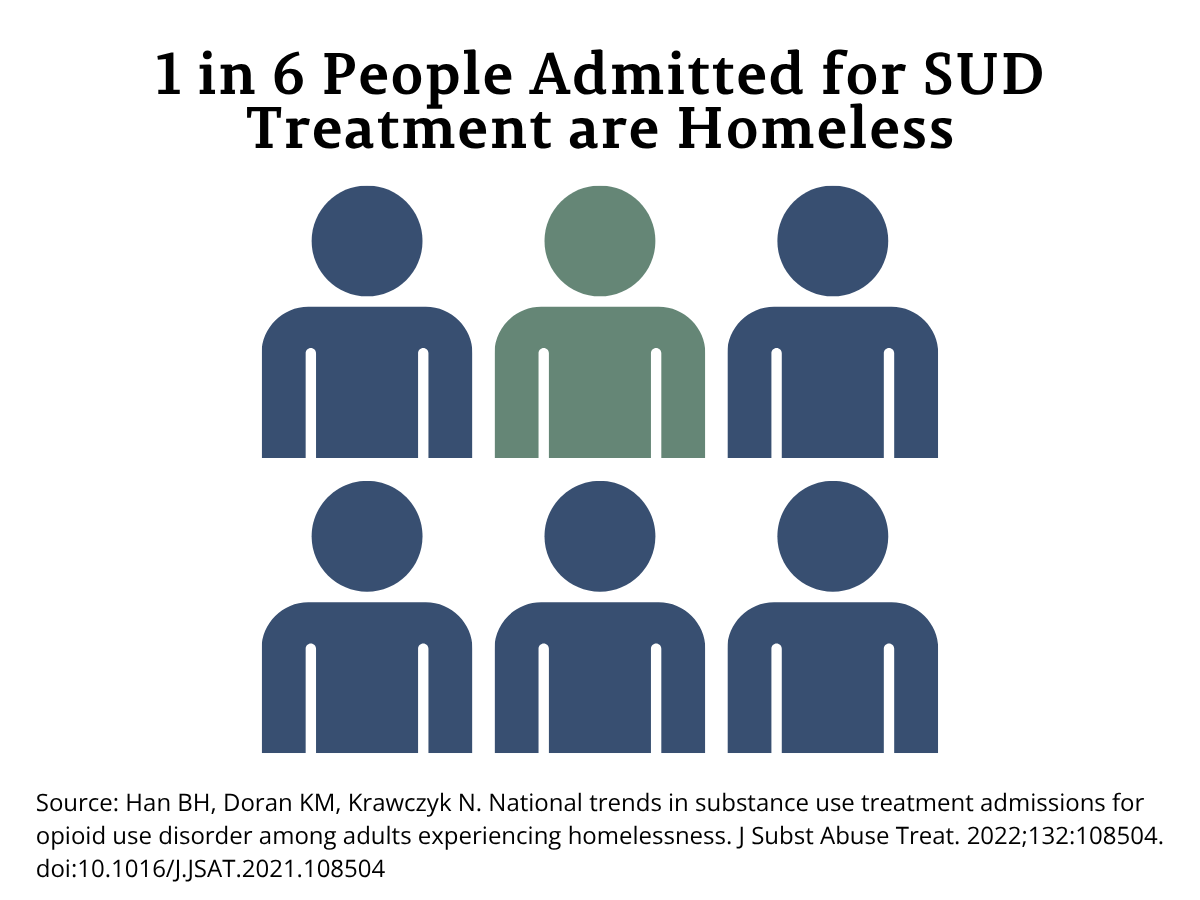
People experiencing homelessness face unique challenges when it comes to substance use and treatment. A 2018 national study found that 16.1% of people admitted for substance use disorder treatment across the United States were experiencing homelessness at the time of admission.59 The same study also showed that completing treatment reduced the likelihood of continued homelessness, highlighting how access to substance use disorder treatment can support stability and recovery.59
Treatment access, however, remains limited. A national study conducted between 2013 and 2017 found that among those entering treatment for opioid use disorder, only about one in four received medications for opioid use disorder.60
In Tennessee, cost remains a significant barrier to lifesaving care. A study of community pharmacies found that high costs often prevent naloxone—an opioid overdose reversal medication—from being distributed more widely.61 Because unhoused individuals are more likely to face financial barriers, they are at greater risk of overdose deaths.
Even with these challenges, research shows that people experiencing homelessness who have substance use disorders are willing to stay engaged in treatment when given the chance.62 This finding reinforces the importance of expanding low-cost, accessible treatment and recovery supports for people without stable housing.
-
Community-Driven Solutions
Community-driven solutions are practical steps local partners can take together to prevent substance misuse and support people affected by it. These actions are evidence-based, can be put in place quickly, and focus on the most urgent needs in each community. Together, they include efforts to prevent substance misuse before it starts and strategies that reduce harm for people who are already using substances.
To reduce substance misuse and its effects, prevention is essential. Communities can help by supporting people early, improving living conditions, and creating stronger connections among neighbors.
For people who are already using substances, it is important to meet them where they are. Substance use carries real and immediate risks, including infection, overdose, and death. Harm reduction is an evidence-based approach that focuses on keeping people alive and as safe as possible while respecting their choices and dignity.
- Naloxone Training & Distribution. Naloxone is a medication that can save someone’s life during an opioid overdose. Anyone can be trained to carry and use it. Health Councils can connect with Tennessee Department of Mental Health and Substance Abuse Services (TDMHSAS) Regional Overdose Prevention Specialists (ROPS), who distribute naloxone and provide training across all 95 counties in Tennessee.
- Fentanyl Test Strip Distribution. Fentanyl is a powerful synthetic opioid that can be deadly in even small amounts and is often mixed with other drugs. Tennessee law allows the use of fentanyl test strips. ROPS are beginning to distribute them—contact your regional specialist to learn more.
- Syringe Services Programs (SSPs). These programs provide sterile needles, safe disposal containers, HIV testing, treatment referrals, education, and other healthcare services. Health Councils can spread awareness of SSPs in their community. In Tennessee, SSPs currently operate in 14 counties (Campbell, Claiborne, Cocke, Davidson, Dyer, Greene, Hamilton, Hancock, Hawkins, Knox, Robertson, Shelby, Union, and Washington Counties) —contact your nearest location to connect with existing programs.
- Safe Medication Storage & Disposal. Simple steps, like locking up medications and properly disposing of unused prescriptions, can prevent misuse before it starts. Health Councils can partner with pharmacies, schools, and law enforcement to distribute lock boxes or promote the installation of permanent drop boxes in the community.
- Count It, Lock It, Drop It or Take Back Day Events. This is a statewide public awareness campaign to promote responsible medication management. These events provide communities an opportunity to properly dispose of unused medication and help educate communities about accidental or recreational misuse.
- Promote the Tennessee REDLINE (1-800-889-9789). The Tennessee REDLINE is the 24/7/365 resource for substance misuse treatment referrals. Share information about REDLINE through social media, newspapers, radio, and local businesses. The more people are aware of these services, the more likely they are to utilize them.
- Change the Language Campaign. The language we use around substance use can either support or stigmatize people. Supportive language focuses on the person, not the behavior, and recognizes substance use as a health issue, not a moral failing. Health Councils can use tools from Changing the Narrative and the NIH library of terms to reduce stigma and support compassionate care. ROPS can provide training on stigma and compassion fatigue.
- Build Recovery-Friendly Communities. Encourage local businesses, organizations, and faith communities to become “recovery-friendly.” This includes hiring practices that offer second chances, peer mentoring, and creating supportive, stigma-free environments. Health Councils can share success stories and provide resources to help communities get started.
- Community Awareness Campaigns. Public awareness matters. County Health Councils can lead local campaigns that highlight available resources and promote positive messages about prevention and treatment. Utilize social media, local radio, and community events to connect with people where they are.
- Share Real Stories. When people share their genuine experiences with recovery or prevention, it helps others see that change is possible and that seeking help is a sign of strength, not weakness. County Health Councils can work with local media, schools, and community events to highlight these success stories. Sharing real stories of recovery and prevention to inspire others and reduce the stigma surrounding seeking help.
-
Making Change Through Policies and Systems
Policy and system changes play an important role in preventing substance misuse. These evidence-informed actions help create safer, more supportive environments that reduce risk and promote well-being.
- Support Parents Through Education. County Health Councils can help families start honest conversations about alcohol and drugs. Hosting family nights, parent workshops, or sharing simple online resources can make it easier for parents to talk with their kids. Programs that strengthen family bonds, enhance communication, and foster parenting confidence can have a lasting impact in preventing substance misuse.
- Build Protective Factors for Kids. When kids feel supported, connected, and valued, they are much less likely to turn to drugs or alcohol. Mentoring programs, after-school clubs, art classes, and community events all help create those strong, positive connections. County Health Councils can partner with schools, youth groups, and local organizations to make these opportunities available to every child. When young people feel they belong, they are more likely to thrive.
- Expand Access Treatment Options. Medication-Assisted Treatment (MAT) uses safe, proven medicines like buprenorphine, methadone, and naltrexone to help people recover from opioid use disorder and rebuild their lives. However, many people still live far from a treatment center or lack reliable transportation. County Health Councils can help by spreading the word about MAT programs and supporting transportation options through volunteer drivers or community ride programs.
- Promote Coordinated Care Models. People recently released from jail or prison face a higher risk of overdose. Coordinated care, where doctors, counselors, and community partners work together and stay in touch, can help reduce that risk. This person-centered approach focuses on continuous communication, stronger relationships, and better follow-up, which leads to improved health and recovery outcomes.
- Train Local Leaders. Teachers, faith leaders, coaches, and employers often see the first signs that someone might be struggling, but they do not always know what to do next. By offering simple, practical training, County Health Councils can equip these trusted leaders with the tools to recognize early warning signs of substance misuse and connect individuals to local resources for help.
- Offer Trauma-Informed and Compassionate Care Training. Many people who struggle with substance use have experienced trauma. Training healthcare providers, teachers, and community members to recognize and respond to trauma with compassion can make a huge difference. Health Councils can help organize or sponsor these workshops locally.
- Provide Mental Health and Wellness Support. Promoting mental health is an essential part of substance misuse prevention. Health Councils can help expand access to counseling, school-based services, peer-led mental health groups, and stress management programs. Supporting emotional well-being strengthens the whole community.
- Use Data to Drive Change. County Health Councils can collect and share local data on substance use trends, treatment access, and prevention outcomes to inform decision-making. This information shows what is working and where more support is needed. Over time, this data-driven approach helps focus resources where they can have the greatest impact.
-
Community Spotlight
The Health Council Community of Practice (CoP) connects Tennessee Health Councils through shared learning and discussion around health priorities. The links below provide access to recent CoP conversations related to this topic. To learn more about the Community of Practice, click here.
Carter County (August 2024)
Hickman County (November 2024)
Hawkins County (October 2025)Submit your own Community Spotlight! Please email Health.Councils@tn.gov with any relevant stories, resources, or presentations related to this topic.
-
Partners and Resources
Tennessee Resources
Tennessee Department of Mental Health and Substance Abuse Services (TDMHSAS)
- Adolescent Substance Use Disorders Services Program
This program provides treatment and support for youth ages 13–18 who are struggling with alcohol or drug use, or who have both substance use and mental health concerns. Services are offered through outpatient, day, and residential programs that include counseling, education, and family support. These services are available to youth who do not have TennCare coverage or other insurance for substance use treatment. - Certified Peer Recovery Specialist Program
Tennessee’s Certified Peer Recovery Specialist program provides State certification for individuals who provide direct peer-to-peer support services to others who have mental illness, substance abuse, or co-occurring disorders. - Lifeline Peer Project
This initiative aims to reduce stigma related to addiction and increase access to substance abuse recovery supports around the state. There are 10 Lifeline coordinators serving regions statewide and 10 hybrid Lifeline coordinators focusing on rural, distressed counties. - Naloxone Training
This comprehensive online training covers what to do in case of an opioid overdose. It explains the signs of an overdose and steps to take when administering naloxone. - Recovery Housing
Safe, stable, quality, affordable housing is an essential component of recovery from substance use disorder. A directory of recovery housing options in Tennessee is available on the TDMHSAS website. - Recovery Support Services
The Addiction Recovery Program (ARP) offers a variety of services to individuals with issues brought on by their substance abuse. Tennessee residents 18 and older who have a substance use disorder or co-occurring disorder may be eligible based on a formal screening and assessment. - Tennessee Recovery Navigators
Navigators are people in long-term recovery who meet with patients with addiction treatment needs in more than 60 hospitals across the state. Drawing on their own lived experience and training as Certified Peer Recovery Specialists (CPRS), Navigators are highly effective at connecting with patients and helping them enter treatment for substance use disorder. - Tennessee REDLINE 1-800-889-9789
This referral service connects people to addiction. The service is provided by the Tennessee Association for Alcohol, Drug, and other Addiction Services (TAADAS) through a contract with TDMHSAS. - Tennessee Regional Overdose Prevention Specialists (ROPS)
ROPS are located across Tennessee and serve as key contacts for training and education on opioid overdose prevention. They help communities stay safe by providing naloxone and guidance on its use. ROPS come from a variety of backgrounds, including peer nurses in recovery, paramedics, and Certified Peer Recovery Specialists. TDMHSAS currently has 20 ROPS working across 13 regional divisions in the state. - Tennessee Substance Use Prevention Coalitions
These community partners work to reduce dependence on harmful and potentially lethal substances such as prescription drugs, illegal drugs, and alcohol.
Tennessee Department of Health (TDH)
- FindHelpNowTN.Org
This online tool helps users locate substance misuse treatment based on their specific treatment needs, available payment and insurance options, and location. - Overdose Response Coordination Office (ORCO)
ORCO guides statewide overdose response efforts through improved coordination, collaboration, analysis, and advocacy. The office provides targeted community education on prevention, drug screenings at local health departments, and referrals to treatment services. - Syringe Services Programs
This comprehensive harm reduction service provides free sterile needles, syringes, and other injection equipment; safe disposal containers; HIV and viral hepatitis testing and linkage to treatment; overdose prevention and education; referrals to substance use disorder treatment, medical providers, and social services; and HIV, STIs, and viral hepatitis prevention education. - Tennessee’s Drug Overdose Dashboard
This interactive tool contains state, regional, and county-level data on fatal overdoses, nonfatal overdoses, and drug prescribing.
Tennessee Opioid Abatement Council
- The Tennessee Opioid Abatement Council oversees the use of funds from national opioid settlement agreements to fight the opioid crisis across the state. The Council is made up of state and local officials, healthcare providers, law enforcement, and community leaders. It also includes people with lived experience to ensure decisions reflect real community needs. The Council works collaboratively to make sure resources are distributed fairly and effectively, supporting prevention, treatment, recovery, and the reduction of overdose deaths through community and county funding.
East Tennessee State University Addiction Science Center
- The ETSU Addiction Science Center (ASC) works with communities in Central Appalachia to better understand and prevent substance misuse. ETSU ASC conducts research, shares evidence-based prevention and treatment strategies, and provides education and training for health professionals. By combining science with community partnerships, the center helps improve care and support for people affected by substance use
- This mapping tool, developed by NORC at the University of Chicago and East Tennessee State University, lets users measure the strength of substance use recovery ecosystems in every county in the United States. Users can explore county-level maps and create data dashboards to see where additional resources are most needed to support individuals in recovery. Insights from this tool can help target resources and interventions to enhance recovery ecosystems, ultimately improving outcomes.
Tennessee Association of Alcohol, Drug, and Other Addiction Services (TAADAS)
- The TAADAS Clearinghouse is an extensive resource center where readers can access free literature on a range of topics, from drug dependence to mental health to medication-assisted treatment.
Tennessee Rural Health Prescription Takeback Toolkit
- This toolkit from the Tennessee Rural Health Association is a comprehensive guide for communities hoping to address prescription opioid misuse through take-back events, pharmacist interventions, and community education.
- The Substance Misuse and Addiction Resource for Tennessee (SMART) Initiative helps community leaders put evidence-based, cost-effective strategies into action to reduce the harm caused by substance use and the opioid epidemic. SMART provides guidance on managing opioid settlement funding, developing community-specific abatement plans, and securing and overseeing state and federal grants related to addiction prevention and recovery. By supporting local leaders, SMART helps communities take practical steps to address substance misuse and its effects.
To Learn More:
- This initiative, led by The Action Lab at Northeastern University in Boston, works to provide up-to-date, evidence-based information on key issues related to drug use and addiction.
Drug Abuse Resistance Education D.A.R.E.
- D.A.R.E. is a series of classroom lessons led by local police officers that teach children from kindergarten through 12th grade how to make safe, healthy choices. The program helps students resist drugs, alcohol, and other high-risk behaviors while building positive relationships with law enforcement and their community.
Substance Abuse and Mental Health Services Administration (SAMHSA)
- FindTreatment.gov
This website is an anonymous resource for persons seeking treatment for mental and substance use disorders in the United States and its territories. - National Helpline 1-800-662-HELP (4357)
This Helpline provides 24-hour free and confidential help. You can get treatment referral and information about mental health and drug or alcohol use disorders, prevention, and recovery in English and Spanish. - 988 Suicide & Crisis Lifeline
Counselors are available to help with mental health struggles, emotional distress, and alcohol or drug use concerns. - Opioid Treatment Program Directory
This directory provides contact information for treatment programs in every state and U.S. territory.
Support Programs
U.S. Department of Veterans Affairs
- The VA provides a range of treatment options for Veterans facing substance use challenges, including medication, counseling, therapy, and support for related conditions such as post-traumatic stress and depression.
- Adolescent Substance Use Disorders Services Program
 Stout Drive Road Closure
Stout Drive Road Closure