Your patient is a 65-year-old woman from Colorado who presents with a chief complaint
of "shortness of breath". She had been well with an unremarkable past history until
10 days prior to admission when she developed flu-like symptoms including fever, headache,
fatigue, myalgias, nausea, vomiting, and diarrhea. Five days after the onset of symptoms
she developed a nonproductive cough and became progressively short of breath.
Your exam reveals an acutely ill woman with a temperature of 38.3°C, a BP of 90/54
mm Hg, a respiratory rate of 20 breaths per minute and a regular pulse rate of 93
beats per minute. Her lips and fingernails are cyanotic. Examination of her lungs
reveals diffuse inspiratory crackles bilaterally. The intensity of the breath sounds
is diminished.
Laboratory studies are positive for leukocytosis, thrombocytopenia, an elevated
AST and ALT, and a prolonged PT/PTT. D-dimers are elevated and an arterial blood gas
analysis reveals a low PaO2 and a metabolic acidosis. A screen test for influenza
A and B is negative. An admission chest x-ray is shown below.
What is your diagnosis, what test(s) would you order to confirm your suspicions,
and what treatment, if any, do you recommend?
Diagnosis: Hantavirus Pulmonary Syndrome (HPS). In the United States Sin Nombre virus is the primary cause of HPS, especially in the four corners region (Arizona, New
Mexico, Colorado, Utah). The virus is carried by species-specific rodents (deer mouse
for Sin Nombre virus) and is usually acquired by inhaling aerosolized rodent excreta. HPS has an incubation
period of 1-5 weeks and a prodrome (fever, chills, myalgias, headache, nausea, vomiting)
of 3-5 days. The cardiopulmonary phase is characterized by rapid-onset noncardiogenic
pulmonary edema, tachypnea, cough, dyspnea, hypotension and shock and has a high mortality
(~35-50%). The diagnosis can be confirmed by the detection of IgM or rising IgG titers
to hantavirus and/or RT-PCR for detection of viral RNA in blood or tissues. Treatment
is largely supportive, although antivirals (Ribavirin) may provide some benefit. Preventive
measures include rodent control in homes and work areas, use of protective equipment
when cleaning rodent-infested areas, and proper ventilation before cleaning enclosed
areas.
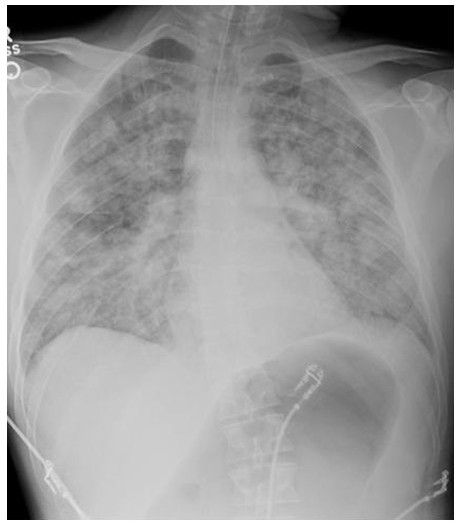
The chest x-ray in HPS mimics the acute respiratory distress syndrome with bilateral interstitial infiltrates progressing to alveolar edema. Pleural effusions (not present in the presented case) may also occur.
 Sam Wilson West Parking Lot C...
Sam Wilson West Parking Lot C...