Medical Mystery of the Week
You are asked to make a diagnosis in this 24-year-old man based on his picture
and a recording of his heart sounds (see below).
DIAGNOSIS: Mitral valve prolapse in a patient with Marfan's syndrome (MFS).
MFS is an autosomal dominant multisystem connective tissue disorder with an estimated
prevalence of one in 3,000 to 5,000 individuals. The primary genetic defect lies on
chromosome 15q21.1 within the coding region for the fibrillin-1 (FB-1) gene. FB-1
is a large glycoprotein produced and secreted by fibroblasts and incorporated into
the extracellular matrix of tissues as insoluble microfibrils. These microfibrils
serve as a scaffold for the deposition of elastin and for the sequestration of latent
transforming growth factor (TGF)-ß thus preventing unregulated stimulation of the
TGF-ß pathway.
Clinical manifestations of MFS may include aneurysmal dilation of the aortic
root (in most instances the ascending aorta and arch maintain their normal dimensions leading
to an "Erlenmeyer flask" shaped aneurysm), aortic rupture or dissection, mitral valve prolapse, cardiomyopathy, arachnodactyl,
scoliosis, pectus deformities, increased joint laxity, enophthalamos, hypertelorism,
ectopia lentis, dural ectasia, spontaneous pneumothorax, and striae atrophica.
The diagnosis of MFS is based on clinical findings, the family history and genetic
testing. MFS patients should have biannual echocardiographic imaging to quantify aortic
root dimensions and mitral valve integrity. They should avoid high impact and isometric
exercises and competetive athletics. The use of beta blockers is contraversial.
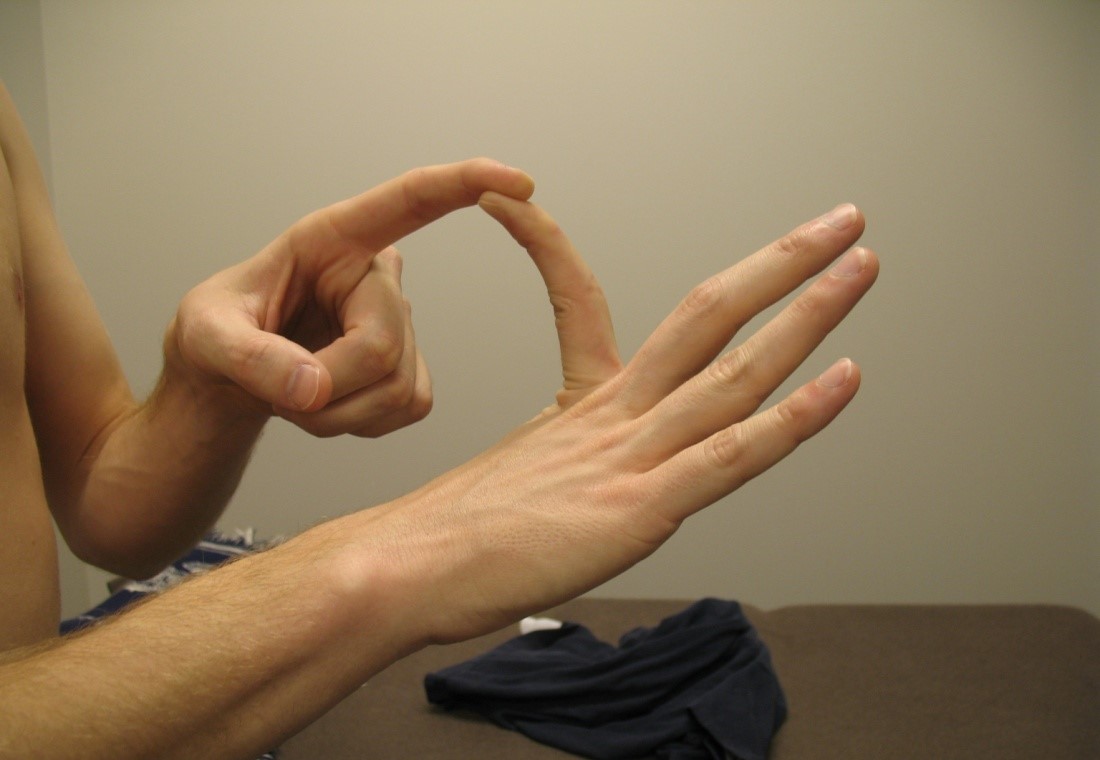
The patient has arachnodactyl and some joint laxity (left image). Systolic and diastolic clicks and a midsystolic murmur are present in the heart recording. These findings are characteristic of mitral valve prolapse (right image).
 Stout Drive Road Closure
Stout Drive Road Closure